Crohn’s disease
What is Crohn’s disease?
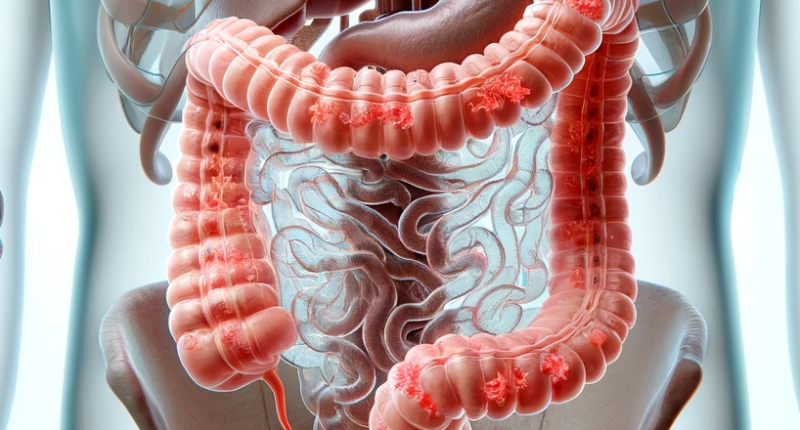
Crohn’s disease is a specific inflammation of the gastrointestinal tract in which granulomas can form anywhere in the gastrointestinal tract. The disease is a chronic, complex systemic lesion of various organs. Severe forms must be treated surgically.
Inflammation of Crohn’s disease develops in and under the mucous membranes. A granulomatous lesion can expand in any area, the preferred localization being in the small intestine, i.e., the ileum. Intestinal damage begins as inflammation of the folds (crypts), from which small “ulcers” form. After that occurs the aphthae – small ulcers. The inflammation penetrates deeper and deeper into the intestinal wall, affecting its size and thickness, i.e., it becomes transmural. The walls thicken, the mobility of the lymph nodes is disturbed, and fistulas can form. The aphthae enhance the formation of a rough scar. During instrumental examination, the intestine’s inner wall has a characteristic “cobblestone” appearance.
The disease begins in adolescence, less often in young people under 35. The course is undulating – periods of calm alternate with periods of exacerbation. There are no gender differences concerning this disease.
People who have relatives with this disease are at risk. In this cohort, the frequency of pathology increases 10-fold. Crohn’s disease is four times more common in smokers than in those who lead a healthy lifestyle. Women who regularly take contraceptive pills are also more likely to get sick.
Symptoms of Crohn’s disease
Symptoms are intestinal and extra-intestinal.
Intestinal:
- frequent loose stools, sometimes so frequent that they disturb sleep.
- abdominal pain of varying intensity;
- reduced appetite;
- nausea and vomiting.
- intestinal blockage;
- drastic weight loss to the point of body mass deficit;
- blood in the stools or intestinal bleeding.
Extra-intestinal symptoms can affect various organs and development associated with autoimmune inflammation. The most common symptoms include the following:
- fever;
- weakness and reduced ability to work;
- abscesses and fistulas within the abdominal cavity, especially extending into the vagina and bladder;
- fistulae, in the pararectal (anal) tissue;
- joint inflammation;
- eye inflammation;
- pustular skin lesions;
- erythema nodosum – dense inflammatory nodules in the vessels;
- inflammation of the gallbladder and liver;
- developmental delay in children if the disease started at an early age.
In addition, one of the main symptoms of the disease is the presence of recurrent fistulas.
Some cases of Crohn’s disease are complicated by dysbiosis, peritonitis, anal fissure or even colon cancer.
Causes of Crohn’s disease
The causes of the disease are not fully understood. Among the main risk factors, doctors call the following:
- hereditary predisposition, which is confirmed by statistics;
- the presence of allergic reactions to various irritants;
- smoking;
- frequent alcohol consumption;
- drug addiction;
- unfavourable ecology.
The primary role in the formation of the disease involves an abnormal reaction of the immune system to your intestinal tissues. For some unknown reason, many white blood cells are sent to the intestinal wall, which becomes the starting point for inflammation.
Diagnosis of Crohn’s disease
The diagnosis of Crohn’s disease in recent decades has become more accurate since the quality and accuracy of medical equipment have improved.
The actual examination and analysis of the clinical picture is performed by a gastroenterologist.
To confirm the diagnosis, the following instrumental studies may be ordered:
- CT of the abdominal organs – fistulas, thickening of the intestinal wall, small abscesses are detected;
- colonoscopy (endoscopy of the mucosa) – detects inflammation, erosions, ulcers, and scars, and allows you to obtain material for biopsy (histological analysis).
- X-ray of the intestine with a contrast – detects changes in structure, narrowing, ulcerative defects, and fistulas;
- capsule endoscopy examines the digestive tract using a capsule that takes pictures through the internal walls.
It is mandatory to apply laboratory diagnostics to the following extent:
- usually a detailed clinical blood test – signs of inflammation and anemia are typical.
- coprogram – stool analysis.
- a fecal occult blood test.
Crohn’s disease treatment.
Treatment is symptomatic, aimed at reducing the symptoms of the disease and mainly conservative.
The basis of treatment is diet. In this diet the amount of fat is reduced, patient can eat crackers, secondary broths, fresh cottage cheese, mashed cooked non-fat meat, soft-boiled chicken eggs, mashed potatoes, porridge, boiled or steamed vegetables, mashed fruit, weak tea, and purees.
Butter products, strong broths, fatty and fried foods, sausages and canned foods, pickles and smoked products, whole milk, legumes, coarse grains, fresh vegetables and fruits, and marinades are prohibited.
The food must be warm, with meals 5-6 times a day. In addition, you need to drink up to one and a half liters of fluid and observe rest.
Alcohol, coffee, strong tea, carbonated drinks, fast food, and smoking are completely ruled out.
Medicines used for exacerbation, anti-inflammatory, immunosuppressants, anti-cytokine and antibacterial agents, and corticosteroid hormones are used as needed.
Hemostatic, painkillers, anti-nausea drugs, laxatives, and vitamins and minerals are prescribed depending on the situation.
Surgical treatment for Crohn’s disease
The main indications for emergency surgical treatment of Crohn’s disease are lack of improvement in the severe course of the disease despite an adequate treatment (including intravenous steroids) for seven days, bowel obstruction due to strictures, fistulas, abscesses, perforation, massive bleeding.
Indications for surgery include severe disease progression with no effect from conservative treatment, frequent exacerbations that significantly impair quality of life, high-grade dysplasia, or carcinoma.
The affected intestine is removed, restoring the patency of the intestine.
All these surgical procedures are performed in more than 750 hospitals all over the world. (https://doctor.global/results/diseases/crohns-disease). For example, proctocolectomy is performed in 25 hospitals in Turkey for a approximate price of $12.9 K. (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/proctocolectomy).
Modern medical advances do not provide a complete cure for Crohn’s disease. However, proper nutrition, curative treatment, and a measured lifestyle can reduce exacerbations and thus improve quality of life. It is essential to give up smoking and alcohol and avoid stress if possible.
Conclusion
Crohn’s disease is a complex and challenging condition that requires ongoing management. While there is no cure, individuals with Crohn’s can lead fulfilling lives by working closely with healthcare providers to develop personalized treatment plans. By understanding the symptoms, diagnosis, and treatment options, those affected by Crohn’s disease can navigate the challenges posed by this chronic condition and enjoy an improved quality of life.