Cervical intraepithelial neoplasia (CIN)
Definition
Cervical intraepithelial neoplasia, or cervical dysplasia, refers to atypical changes of the epithelium in the vaginal part of the uterus, which are related to precancerous processes. In the early stages of its development, cervical dysplasia is a reversible disease, so its timely detection and elimination is a reliable way to prevent cancer risk. Unlike erosion, arising from mechanical trauma to the tissues, dysplasia violations affect the cellular structures of the tissues lining the cervix. The incidence of cervical dysplasia is mainly between 25-35 years of age and is 1.5 cases per 1000 women.
Types of cervical dysplasia
The lower, narrow, cylindrical part of the uterus, partly located in the abdominal cavity and partly extending into the vagina (supravaginal and vaginal part, respectively), is the cervix.
The vaginal part of the cervix is examined using vaginal mirrors during a gynecologic examination. Inside, a narrow cervical canal 1-1.5 cm long runs along the cervix, one end of which (the external pharynx) opens into the vagina and the other (the internal pharynx) into the uterine cavity, connecting the two.
From the inside, the cervical canal is lined with a layer of epithelial cylindrical cells and contains mucus-producing neck glands. The mucous secretion of the cervical canal prevents the entry of microflora from the vagina into the uterus. The epithelial cylindrical cells are bright red.
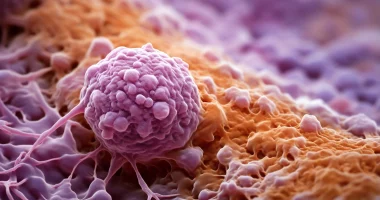
Abnormalities in the structure of cells and layers of squamous epithelium characterize cervical dysplasia. Altered epithelial cells become atypical—large, shapeless, with multiple nuclei, and the separation of epithelium into layers disappears.
Cervical dysplasia can affect different layers of squamous epithelial cells. There are 3 degrees of cervical dysplasia depending on the depth of the pathological process. The more layers of the epithelium are affected, the more severe the degree of cervical dysplasia. According to the international classification, there are distinguished:
- Mild cervical dysplasia (CIN I): Changes in cell structure are weakly expressed and affect the lower third of the multilayer squamous epithelium.
- Moderate cervical dysplasia (CIN II) – changes in cell structure are observed in the lower and middle thirds of the squamous epithelium.
- Severe cervical dysplasia or non-invasive cancer (CIN III): Pathological changes are found throughout the thickness of epithelial cells but do not spread to vessels, muscles, or nerve endings, as in invasive cervical cancer, which affects these structures.
Causes
The most common causes of cervical dysplasia are oncogenic types of human papillomavirus (HPV-16 and HPV-18). This cause is detected in 95-98% of patients with cervical dysplasia. With prolonged presence in the body and cells of squamous epithelium (1-1.5 years), papillomavirus infection causes changes in the structure of the cells, i.e., dysplasia. Some aggravating background factors contribute to this:
- immunodeficiency – suppression of immune reactivity by chronic diseases, stress, medications, improper diet, etc.;
- active and passive tobacco smoking – increases the likelihood of developing cervical dysplasia by four times;
- prolonged chronic inflammation of the genitals;
- hormonal disorders caused by menopause, pregnancy, use of hormone-containing drugs;
- early sexual activity and childbirth;
- traumatic injuries to the cervix.
Symptoms of cervical dysplasia
Cervical dysplasia has almost no distinctive clinical picture. A latent course of dysplasia is observed in 10% of women. Much more often, cervical dysplasia is joined by microbial infection, causing pathological symptoms of colpitis or cervicitis: burning or itching, discharge from the genital tract of unusual color, consistency, or odor, sometimes with an admixture of blood (after using tampons, sexual intercourse, etc.). Painful sensations in cervical dysplasia are almost always absent. Cervical dysplasias can have a long course and regress independently after appropriate treatment of inflammatory processes. However, the process of cervical dysplasia is usually progressive.
Cervical dysplasia often occurs together with diseases such as acute condylomas of the vagina, vulva, anus, chlamydia, and gonorrhea.
The absence of obvious clinical symptoms in cervical dysplasia brings instrumental, clinical, and laboratory techniques to the forefront of diagnosis.
Diagnosis of cervical dysplasia
The diagnostic scheme for cervical dysplasia consists of:
- examination of the cervix using vaginal mirrors – to detect visible, clinically expressed forms of dysplasia (change in the color of the mucosa, shine around the external pharynx, spots, overgrowth of the epithelium, etc.);
- colposcopy – examination of the cervix with a colposcope – an optical apparatus that magnifies the image more than ten times and simultaneous diagnostic tests – treatment of the cervix with Lugol’s solution and acetic acid;
- cytologic examination of PAP smear – in the case of cervical dysplasia, microscopic examination of the scrapings obtained from different sites allows for the detection of atypical cells. The PAP smear also detects marker cells of papillomavirus infection, which have shriveled nuclei and a rim that are the localization site of the human papillomavirus;
- histologic examination of a biopsy – a fragment of tissue taken during a cervix biopsy from the area suspected of dysplasia. It is the most informative method for detecting cervical dysplasia;
- immunologic PCR methods – to detect HPV infection, to determine the strain of the virus and viral load (concentration of papillomavirus in the body). Detection of the presence or absence of oncogenic HPV types helps to determine the choice of treatment method and management of a patient with cervical dysplasia.
Treatment of cervical dysplasia
The choice of treatment for cervical dysplasia is determined by the degree of dysplasia, the woman’s age, the size of the affected area, comorbidities, and the patient’s intentions to preserve fertility. The leading place in the treatment of cervical dysplasia is occupied by:
- Immunostimulatory therapy (immunomodulators, interferons, and their inducers) is indicated in the case of extensive lesions and the course of cervical dysplasia, which is prone to recurrence.
- Methods of surgical intervention:
- Destruction (removal) of the atypical area using cryotherapy (exposure to liquid nitrogen), electrocoagulation, radio wave therapy, argon or carbon dioxide laser;
- surgical removal of the area of cervical dysplasia (conization) or the entire cervix (amputation).
If the degree of dysplasia I and III, the small size of the altered area, and the patient’s young age, a wait-and-see approach is often chosen because of the high probability of cervical dysplasia regressing on its own. Conducting repeated (every 3-4 months) cytologic studies and obtaining two positive results confirming the presence of cervical dysplasia is an indication to address the issue of surgical treatment. Treatment of dysplasia IIІІІ is performed by gynecologic oncologistsusing one of the surgical methods (including cone-shaped amputation of the cervix).
Before any of the surgical methods for treating cervical dysplasia, a course of anti-inflammatory therapy is prescribed aimed at sanitizing the infectious focus. As a result, the degree of cervical dysplasia is often reduced or eliminated.
All these treatment options are available in more than 730 hospitals worldwide (https://doctor.global/results/diseases/cervical-intraepithelial-neoplasia-cin). For example, Conization can be done in 25 clinics across Turkey for an approximate price of $1.6 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/conization).
Rehabilitation after treatment
After surgical treatment of cervical dysplasia, the rehabilitation period lasts about four weeks. During this time, you may experience:
- aching pain in the lower abdomen for 3-5 days (longest after laser destruction);
- discharge from the genital tract – abundant, sometimes with odor for 3-4 weeks (the longest – after cryodestruction);
- profuse, prolonged bleeding from the genitals, intense pain in the lower abdomen, and a rise in body temperature to 38 ° C or higher – are indications for immediate medical consultation.
To recover as soon as possible, faster healing, and prevent complications, it is necessary to observe sexual rest, the exclusion of sprinkling, lifting weights, the use of hygienic tampons, and accurate fulfillment of all recommendations and prescriptions of the doctor.
Surveillance and prevention of cervical dysplasia
The first cure check of cervical dysplasia is performed 3-4 months after surgical treatment. Cytologic smears are taken, followed by quarterly repeats for a year. Negative results showing the absence of cervical dysplasia allow further examination in a routine manner at annual dispensary examinations.
To prevent cervical dysplasia and its recurrence, it is recommended:
- inclusion in the diet of all micronutrients and vitamins, especially vitamins A, B group, and selenium;
- timely sanitation of all foci of infection;
- tobacco cessation;
- use of barrier contraception (in case of casual sexual contacts);
- regular gynecological follow-up (1-2 times a year) with examination of cytologic scrapings from the cervix.