Knee Osteoarthritis
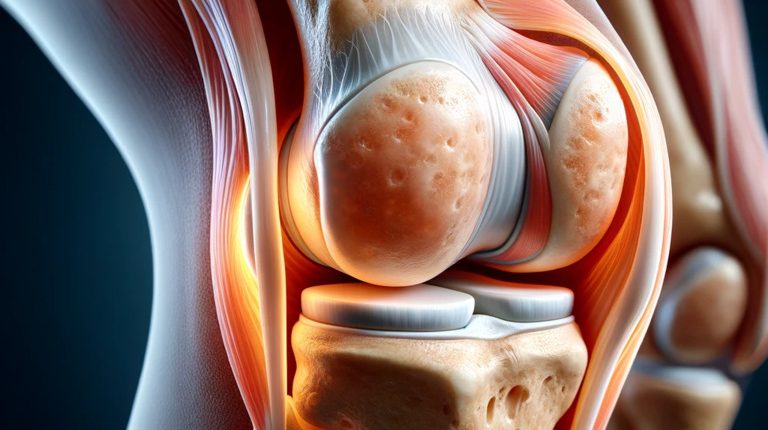
Knee osteoarthritis, or gonarthrosis, is a dystrophic lesion of the cartilage tissue of the knee joint that leads to degeneration and secondary reaction of the bone tissue.
Disease
What does gonarthrosis mean? One of the most common forms of chronic degenerative-dystrophic diseases is osteoarthritis of the knee joint, in which the synovial membrane, articular cartilage, and other joint structures are involved. This pathology is characterized by a long progression and development of a pain syndrome. Osteoarthritis often causes long-term health problems and has negative psychological and economic effects on patients.
Diagnosis of the disease in the early stages is based on the results of an ultrasound examination of the joint. Radiography allows you to assess the condition of the bone tissue and its involvement in the pathological process. In complex clinical cases, computer or magnetic resonance imaging and endoscopic surgery are used.
According to clinical guidelines, knee osteoarthritis treatment is determined by the stage of the pathological process. In the early stages of the disease, conservative treatment is effective, including intra-articular drug administration, and in the late stages, the issue of surgical intervention is resolved. The consequences of gonarthrosis can be complete immobilization of the joint and subsequent disability, so timely treatment is essential.
Classification
Osteoarthritis of the knee is classified into two types:
- primary, which is often due to genetic characteristics of knee structures;
- secondary, which develops in the presence of a predisposing disease or condition (diabetes, trauma, etc.).
In first-degree gonarthrosis, there is an initial process of thinning of the cartilage plate. The second degree is characterized by narrowing the joint gap, and bone osteophytes also occur. In the next stage, the space between the joint ends significantly narrows in places where the bone is exposed. In the fourth degree, the joint separation is absent; the joint is damaged.
Symptoms of gonarthrosis
The main symptoms of gonarthrosis include:
- mechanical nature of the pain – occurs or increases with the load on the knee, in the evening at rest the pain subsides, and at night usually completely stops;
- morning stiffness – a person needs up to half an hour for knee to stop aching;
- a limited range of motion that involves both a reflex without sparing the joint in response to pain and a mechanical block;
- limited activities, such as difficulty putting on socks and shoes.
Target signs of knee osteoarthritis include:
- presence of pain along the edges of the joint (tenderness when palpating the periarticular tissues);
- the appearance of minor thickenings at the edges of the joint;
- a rough crack during motion, as well as the appearance of a joint jamming symptom;
- moderate inflammatory signs that are caused by secondary synovitis (cold fluid accumulation in the knee);
- feeling of tension in the knee joint;
- knee instability, which indicates severe cartilage degeneration.
Causes of gonarthrosis
Causes of gonarthrosis may include the following:
- High body mass index and low physical activity of the patient. Obesity increases the load on the knee joint during walking and indirectly affects the unloaded parts of the joint due to the systemic action of pro-inflammatory cytokines. Obesity increases the likelihood of developing gonarthrosis by 4-10 times and occurs in one in three patients.
- Diabetes mellitus. The cartilage plate at the joint ends of the bone, the ligamentous compartment, and the subcartilage area of the bone receive nourishment only from the oxidation of glucose. Therefore, insufficient intake of this substance within the cells causes metabolic disorders to be triggered.
- Gender. Women are at higher risk than men, mainly after the onset of menopause.
- Age. The older a person is, the greater the likelihood of degenerative-dystrophic damage to the cartilage of the knee joint.
- Physical activity. Knee is not well affected by both exercise and physical hard work (loaders, powerlifters, etc.). Optimal (moderate) physical activity should be maintained to sustain joint health.
- Joint injuries. Post-traumatic changes create a background of accelerated cartilage degeneration.
- Vitamin D deficiency. Studies have shown that this substance is actively involved in maintaining the health of articular cartilage.
- Tobacco smoking. Nicotine and burning products lead to vascular spasms, depriving poorly vascularized cartilage sheets of nutrition.
- Strength of the quadriceps femoris. Weakness of the quadriceps femoris is a risk factor for the development and progression of osteoarthritis, especially in women. Usually, the strength of the quadriceps muscle in women is usually two times lower than in men (72.0 vs. 125.7 N/cm2), significantly affecting joint stability. Training for five weeks, including 30 minutes of exercise, statistically significantly increases muscle strength, improves joint function, and reduces the severity of pain. Training results are saved for six months if you exercise for 20-30 minutes daily.
It is believed that the development of degenerative-dystrophic processes in gonarthrosis is associated with a disturbance of microcirculation in the articular ends of the knee joint. In this case, the severity of the pathological process is proportional to the degree of circulatory disturbances in the cartilaginous layer of the bone epiphyses.
Diagnostics
The following visualization diagnostic methods can be used to evaluate the knee joint:
- radiography;
- ultrasound scanning;
- computed tomography;
- magnetic resonance imaging;
- arthroscopic surgery (an invasive procedure involving the insertion of an arthroscope for examination of the joint cavity and evaluation of its condition under magnification).
Treatment of gonarthrosis
Treatment of gonarthrosis depends on the stage of the disease and is based not only on objective research methods but also primarily on the subjective feelings of the patients. Conservative treatments, such as intra-articular injections, are most effective in the early stages of gonarthrosis. Arthroscopy of the knee joint can achieve a significant effect if applied relatively early (stage II-III). Knee arthroplasty is the gold standard treatment for patients with stage III-IV gonarthrosis.
Conservative treatment
Conservative treatment of osteoarthritis gives positive results in the first and second stages of the disease. The main principles of conservative treatment are pain relief, elimination of causes that contribute to disease progression and restoration of lost functions, and prevention of complications of gonarthrosis.
For pain relief, non-steroid anti-inflammatory drugs, which can be used both systemically and topically in the form of creams or gels, are most commonly used. The most popular medications for intra-articular management are hyaluronic acid, platelet-rich plasma, and corticosteroids. Intra-articular administration of hyaluronate is very effective in the early stages of the disease, reducing pain and improving limb function. Injections of high-purity hyaluronic acid can increase the viscosity of the synovial fluid and the absorption of compressive forces. On average, the positive effect lasts for six months or more.
Increasingly, platelet-rich plasma containing various proteins and growth factors that can enhance tissue repair is used to treat diseases and injuries of the musculoskeletal system. Osteoarthritis is the main indication for this treatment. Studies have confirmed the absence of complications after such treatment.
Physiotherapy for osteoarthritis has been used for a long time. In addition to classical methods (magnetic therapy, electrophoresis, etc.), there are new ones. The use of low-frequency magnetic light therapy can significantly relieve pain. Recently, ways to reduce the load on joints, using orthoses or tapes, have been successfully used, especially with only one joint component osteoarthritis.
Surgical treatment
In most cases of gonarthrosis, three main methods of surgical intervention are used for the surgical treatment of gonarthrosis. These include endoscopy, corrective osteotomy, and endoprosthetics. Arthroscopic interventions are frequently performed and can be of varying amounts (revision and removal of necrotic fragments, laser coagulation, cartilage plate plastic surgery).
In the most severe cases, more invasive techniques are also used – from corrective osteotomies to endoprosthetics. Corrective osteotomy is the most effective and is indicated as an initial step in breaking the axial parameters of the limb. In advanced cases, taking into account the full range of medical and social factors, in addition to endoprosthetics, arthrodesis – an operation of desperation – may sometimes be recommended.
All these surgical procedures are performed in more than 980 hospitals worldwide (https://doctor.global/results/diseases/knee-osteoarthritis). For example, arthroscopic chondroplasty is done in 43 clinics across Germany for approximate price of $13.1 K (https://doctor.global/results/procedures/arthroscopic-chondroplasty).
Prevention of gonarthrosis
The main direction for the prevention of gonarthrosis is adequate physical activity. The positive role of moderate exercise in the combined treatment of osteoarthritis is not limited to weight loss – it also increases joint stability and improves vascularization, stimulating the synthesis and remodeling of joint cartilage components that arrests disease progression. Physical activity aimed at strengthening the hip quadriceps also plays an important role.
Rehabilitation
After surgical treatment for knee osteoarthritis, rehabilitation is essential. The patient is advised to monitor the load on the joint, do physical therapy exercises, undergo physical therapy procedures, monitor weight, and treat primary medical conditions.