Liver metastases
What’s that?
Liver metastases is a secondary form of cancer when malignant cells spread through the blood and lymphatic systems from the main focus of the lesion, located in another organ. The most common carriers of primary oncology are the lungs, stomach, prostate, breast, and uterus. Despite the seriousness of this form of cancer, modern medicine makes it possible to significantly increase the duration and quality of life of patients with metastatic liver cancer.
Reasons
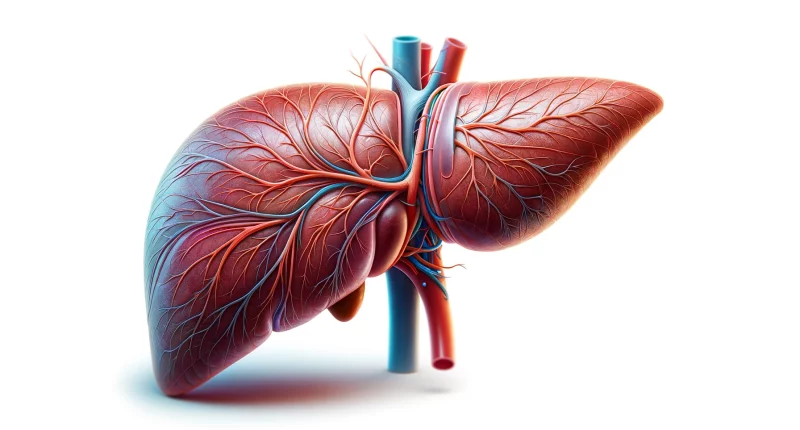
The reason cancer metastases are more likely to spread to the liver than to other organs is due to its anatomy and unique functions. The liver plays a vital role in cleansing the body and can pass up to one and a half liters of blood every minute. When cancer cells spread through the bloodstream, they pass through the liver, where new tumors can eventually form. The rate at which they appear depends on how aggressive the primary tumor is.
Metastatic liver cancer develops in the following cases:
- late diagnosis of primary cancer, lack of treatment, or poor-quality cancer care;
- advanced stage III or IV cancer of the lung, stomach, colon, pancreas, and other organs;
- smoking, alcohol abuse.
Classification
Depending on the number, metastases are:
- singular or solitary;
- sporadic (up to 10);
- multiple (more than 10).
Depending on the size, metastases are represented by:
- small (up to 1 centimeter in diameter);
- medium (1-3 centimeters);
- large (over 3 centimeters).
Symptoms of liver metastases
The following manifestations accompany secondary liver cancer:
- abdominal bloating with a feeling of discomfort;
- nausea with vomiting;
- constipation or diarrhea;
- decreased appetite;
- drastic weight loss;
- general malaise and rapid fatigue;
- slight but persistent increase in body temperature.
Unfortunately, these signs of liver metastases are not specific and unique to oncologic pathologies. This means these manifestations can easily be confused with symptoms of other liver disorders. This fact complicates the diagnosis of this disease and reduces the probability of making the correct diagnosis. However, experts always remember that secondary foci of cancer in the liver tissue are one of the most frequent options for the spread of metastases in many types of malignant pathologies.
Gallbladder disruption is also a prevalent symptom of metastases to the liver. As the size of the secondary focus of the cancerous tumor grows, the bladder gradually constricts its biliary tract. And this, to an increasing extent, makes it more and more challenging to outflow bile into the intestinal cavity. The patient, at this stage, begins to develop mechanical jaundice. It is because the bile, unable to be removed from the gallbladder naturally, enters the bloodstream through its walls. Then, with the bloodstream, it is spread throughout the body, which leads to a characteristic jaundiced coloration of the skin, protein and mucous membranes of the eye, and lightening of feces in humans.
Urine, on the other hand, takes on a dark color. In addition, the chemical effect of bile acids causes itching on the skin. At the same stage of the development of the disease, patients begin to complain of constant aching pain in the right subcostal region. It is due to an increase in pressure in the gallbladder.
Further, a dense lumpy neoplasm begins to be palpable in the right subcostal region at the late stages of malignant tumor development. Liver metastases at this point already become the cause of anemia, spontaneous bleeding from internal organs, and ascites, i.e., accumulation of fluid in the abdominal cavity. Finally, the liver as a whole gradually loses its ability to neutralize various dangerous chemicals, and the patient’s condition deteriorates further due to increasing intoxication of the body.
Diagnosis of liver metastases
Oncological specialists use the full range of modern laboratory and instrumental techniques to detect this pathology. In particular, secondary foci of cancerous tumors can be visualized with the help of:
- ultrasound;
- radioisotope scans;
- computer, magnetic resonance, and positron emission tomography combined with computed tomography.
The detection of a cancer marker called alpha-fetoprotein (AFP) in the patient’s blood plays a vital role among the methods for diagnosing liver cancer. This marker is a protein compound typically present only in the fetus’s bloodstream and disappears after birth. The appearance of AFP in the blood of an adult is evidence of the development of tumorigenesis in the liver. The final confirmation of the diagnosis of secondary liver cancer is made by biopsy of the tumor focus.
Metastatic liver cancer is not divided by stage. By the international classification TNM, the presence or absence of metastases in distant organs reflects the parameter “M.” Regardless of where the primary tumor originated, the appearance of its metastases in other organs is classified as “M1” and automatically transfers the disease to stage IV. Thus, if the primary tumor has already metastasized to the liver, it is, in any case, stage IV cancer.
How to treat liver metastases
The choice of the optimal treatment scheme for this pathology depends on the size of the secondary cancer focus, the exact location of its localization, and the patient’s age and general condition. The treatment regimen for metastatic lesions is developed taking into account several factors:
- whether single or multiple metastases have been identified;
- if there’s metastasis to the lymph nodes;
- whether they are located in the periphery or near large blood vessels and bile ducts;
- histologic type of tumors.
Surgical intervention
The most radical and, at the same time, effective way to get rid of liver metastases is surgical intervention. It involves removing the part of the liver where the secondary focus was detected. If the size of the tumor is large, it may require resection of half of the organ. In this case, the ability of the organ to regenerate plays a significant positive role. Therefore, even with a solid metastatic lesion of the liver with cancer cells, it is possible to remove cancer foci in several stages.
The method of intervention can be either traditional, with broad access through the abdominal wall, or laparoscopic. The second method is preferable due to less traumatization of the patient’s tissues, but it can be used only in single and small metastases. It is possible in 5-20% of all cases. A laser cyberknife is used for metastases up to 1 mm in size.
Chemotherapy for liver metastases
Chemotherapy with cytostatic drugs for liver metastases blocks the growth of cancer cells and their division. It slows down or completely stops the development of the metastatic tumor. Often, this method reduces the volume of neoplasm and makes inoperable metastatic focus operable.
In clinical practice, the liver often deactivates many chemo medications. In this case, chemoembolization is performed – a chemo drug is injected into the metastasis vessel with a substance to occlude the vessel. In any case, traditional cytostaticdrugs in secondary tumor lesions of the liver rarely demonstrate efficacy. Nevertheless, international treatment protocols sometimes recommend the use of polychemotherapy with several medications. Their choice depends mainly on the type of tumor that is primary.
In addition, targeted therapy is widely used today. It uses drugs with a specific action target – a particular molecule necessary for the growth and survival of cancer cells. Sorafenib is the most common targeting drug for metastatic liver cancer.
Radiation therapy
Modern radiation therapy techniques are highly precised – this increases the effectiveness of treatment and minimizes the risk of recurrence. Their goal is to destroy cancer cells without affecting healthy cells. In case of liver metastases, intense, focused radiation, isotope radiation with hepatic vein bypass, or radiofrequency hyperthermia are used.
Other methods
If the clinical situation allows, radiofrequency ablation is performed – malignant masses are destroyed by a high-frequency current delivered from a needle electrode through a puncture in the skin. Another promising experimental treatment method is the destruction of liver metastases by ultrasound waves.
In addition to specific anti-cancer therapy for liver metastases, hepatoprotective treatment is indicated to prevent toxic damage to the organ. It aims to normalize liver parameters – ALT and AST, gamma-glutamyltransferase, bilirubin, and alkaline phosphatase. By indications, detoxification is also carried out. If metastases to the liver violate protein synthesis, the body is supported by the introduction of protein preparations.
In addition, several other modern techniques can be used to treat liver metastases:
- radiosurgery;
- selective internal radiation to the tumor site (SIRT);
- proton and thermal exposures;
- transcatheter embolization of tumor sites;
- implantation of chemotherapy infusion port systems into the liver vessels.
All these treatment options are performed in more than 860 hospitals worldwide (https://doctor.global/results/diseases/liver-metastases). For example, chemoembolization is done in 14 clinics across Turkey for an approximate price of $6.2 K (https://doctor.global/results/procedures/chemoembolization).
Complications of metastatic liver cancer
The most frequent complication of secondary tumor foci in hepatic tissue is the sprouting of neoplasm into the gallbladder and biliary tract, which is manifested by pain sensations in the upper and right abdomen, blunt and constant.