Congenital heart defects (CHDs)
What’s that?
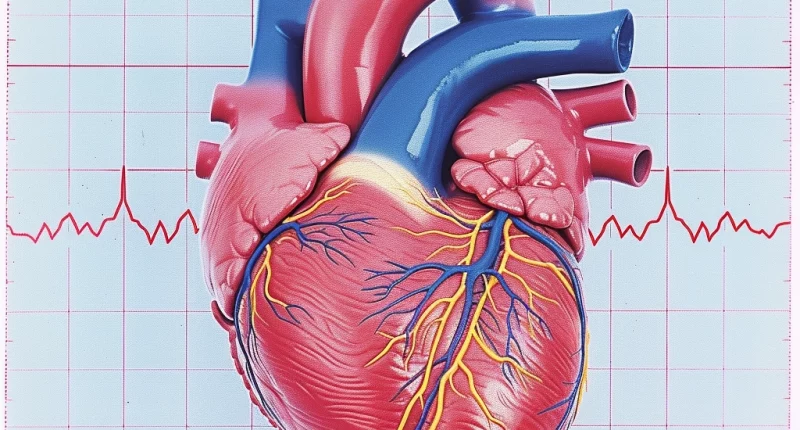
A heart defect is an anomaly of the structure of this organ, which, to a greater or lesser extent, affects its work. It can be congenital or occur during the patient’s life under the influence of certain factors. Depending on the type and stage of heart defects, they may be subject to dynamic monitoring and require symptomatic drug treatment or urgent surgical correction. Once this occurs, it sooner or later leads to severe heart failure, so patients suffering from this pathology need to be monitored by a doctor.
About the disease
Heart defects in adult women and men are more often categorized as acquired since congenital anomalies as the child grows either cure themselves, undergo surgical correction, or lead to the death of the patient.
The normal structure of the heart ensures the separation of arterial and venous blood flows and sufficient blood supply to tissues, supplying them with the necessary amount of oxygen and other nutrients. In malformations, these mechanisms are disturbed, and the load on certain parts of the organ (depending on the type of pathology) increases – its dysfunction develops, organs and tissues experience oxygen starvation, which affects the patient’s well-being and is manifested by the corresponding symptomatology.
Types
First of all, a distinction is made between congenital defects (formed in utero) and acquired defects (caused by external factors in the course of the patient’s life).
Depending on the peculiarities of hemodynamics, congenital malformations can be “white” (when venous and arterial beds do not mix) and “blue” (venous blood enters the arterial bed and spreads throughout the body, the organs and tissues experience oxygen deficiency, the patient has cyanosis – a bluish tint of the skin, which gives rise to the name).
Depending on the type of defect, the heart septum, blood vessels, or valves may be affected. Acquired malformations are valve malformations affecting the mitral, tricuspid, aortic, and pulmonary artery valves, and are of two types:
- stenosis (narrowing) of the valve, in which a sufficient amount of blood is not delivered to the other part of the heart during its contraction, and more blood than physiologically necessary accumulates in that part of the heart;
- insufficiency, in which during the phase of myocardial relaxation through insufficiently closing valve flaps, part of the blood flows in the opposite direction – from the underlying section to the overlying section.
If both stenosis and insufficiency of the same valve are detected simultaneously, the defect is called combined, and if several valves are affected simultaneously – concomitant.
A defect not accompanied by signs of circulatory failure is considered compensated, characterized by circulatory failurein certain situations (e.g., with intense physical activity) – sub-compensated, proceeding with constant symptoms of heart failure – decompensated.
The classification of heart defects proposed by the New York Association of Cardiac Surgeons, which makes it possible to assess the degree of severity of changes in the organ and determine the need for surgery, is of practical use. According to this classification, there are four classes of defects:
- 1 – there is a defect, but there are no pronounced changes in the heart structure, clinical manifestations of pathology are absent, surgery and active drug treatment are not required;
- 2 – changes in heart structures and clinical manifestations of pathology are present, but they are insignificant and reversible; surgery with a predicted 100% success rate is recommended for correction;
- 3 – irreversible changes in the structure of the heart are determined, but the processes in the body caused by them and clinical manifestations of pathology are reversible; surgical intervention is likely to help correct the defect and improve the patient’s condition, but its benefit-risk ratio is determined individually in each specific situation;
- 4 – the defect has led to irreversible changes in the heart and other organs of the patient; surgical intervention is inappropriate and ineffective.
Symptoms
Heart defects in adults are characterized by symptoms such as these:
- general weakness, rapid fatigue;
- episodes of dizziness, fainting;
- frequent, prolonged infectious diseases;
- palpitations, a feeling of interruptions in the work of the organ, heaviness, pain behind the sternum;
- dyspnea – at first during physical activity, then at rest, especially when lying on the back;
- cough;
- pale skin;
- swelling – first in the feet, ankles, and shins, gradually occupying a larger and larger area of the body, spreading from bottom to top;
- heaviness, dull pain in the right subcostal region;
- in the decompensation stage – an increase in the size of the abdomen due to the accumulation of pathological fluid in it (ascites);
- in case of long-term existence of the pathology – signs of chronic hypoxia (thickening of the terminal phalanges of fingers like “drumsticks,” deformation of nails like “hourglasses”).
Reasons
Congenital anomalies arise due to gene mutations or as a result of exposure of the mother’s body, and through it – and the fetus, unfavorable factors:
- infections (rubella, chickenpox, and others);
- radiation;
- nicotine, alcohol, drugs;
- certain drugs and medications;
- industrial toxins, and poisons.
Causes of acquired heart defects:
- infections (streptococcal acute tonsillitis, influenza virus, enterovirus, and others) affecting the endocardium;
- autoimmune processes in systemic lupus erythematosus and other systemic connective tissue diseases;
- aortic aneurysm;
- atherosclerosis;
- coronary artery disease;
- hypertension.
Diagnosis
Identifying the signs and treating heart defects in adults is handled by a cardiologist or cardiac surgeon.
The diagnostic process includes:
- Careful collection of complaints.
- Clarification of data on the history of the current disease and the patient’s life.
- Objective examination (measurement of height, weight, blood pressure, pulse, examination with assessment of skin condition, determination of the degree of swelling of tissues, listening to cardiac activity, verification of murmurs, percussion of borders to determine the organ’s size).
Additional research methods:
- electrocardiography;
- Holter ECG monitoring;
- Cardiac ultrasound (electrocardiography) with Doppler ultrasound;
- chest X-ray;
- in complex diagnostic situations – computed or magnetic resonance imaging;
- clinical blood test;
- Biochemical blood tests (glycemia, rheumatoid tests, and other indicators).
Treatment
Some patients with diseases in this group need only dynamic monitoring. Others may require symptomatic drug treatment or surgical correction of the damaged part of the organ.
Drug therapy usually includes drugs from these groups:
- antihypertensive drugs;
- diuretics;
- antiarrhythmics;
- cardiac glycosides;
- cardiometabolics, cardioprotectors;
- anticoagulants, antiplatelet drugs;
- antibiotics;
- in autoimmune nature of the pathology – glucocorticoids and cytostatics.
The type of surgical treatment depends on the type and severity of the heart defect:
- in case of stenosis – commissurotomy (separation of fused or scarred valve flaps, enlargement of the opening between heart sections, allowing to improve hemodynamics);
- In case of insufficiency, prosthesis, or repair of the existing valve;
- in case of combined defects – replacement of the affected valve with an artificial one, sometimes with commissurotomy;
- in case of combined malformations – one-stage valve replacement.
Modern heart surgeries are, as a rule, minimally invasive interventions – they are performed through a catheter inserted through the vascular access into the heart. It improves patient tolerance, minimizes the risk of complications, and shortens the recovery period.
All these treatment options are available in 770 hospitals worldwide (https://doctor.global/results/diseases/congenital-heart-defects-chds). For example, Rashkind procedure is performed in 8 clinics across Turkey for an approximate price of $7.2 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/rashkind-procedure).
Prevention
Reducing the risk of developing acquired heart defects can help:
- timely treatment of infectious diseases to prevent the spread of infection to the heart or chronification of pathology;
- adequate treatment of autoimmune diseases and metabolic pathology, achieving a stable remission;
- rational, balanced nutrition;
- minimizing stress;
- adequate sleep;
- active lifestyle, daily physical activity in the amount of at least walking;
- avoidance of bad habits (smoking, drinking alcohol, taking drugs).
Rehabilitation
Patients who have undergone surgical intervention to correct a valve defect need thorough dynamic monitoring by a cardiologist or cardiac surgeon to monitor the functioning of their own and/or artificial valves, the quality of cardiac activity, and the timely correction of emerging disorders. Patients are also prescribed supportive treatment, including primarily anticoagulants, if necessary – drugs and other groups.