Synovitis
What’s that?
Synovitis is a joint disease of an inflammatory nature in which the synovial membrane is affected.
About the disease
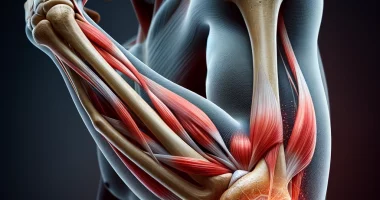
The synovial membrane is the inner sheath of the joint capsule, tendon sheaths, and joint sockets. It produces a viscous synovial fluid that protects the anatomical structures from excessive friction and facilitates their gliding.
Symptoms of synovitis are the classic signs of inflammation. There is pain, swelling, and limited function in the affected area. Palpation is determined by an increase in local temperature, with reddening of the skin in the area of inflammation.
In almost every second case, synovitis is associated with osteoarthritis, i.e., synovial inflammation is reactive. But synovitis can also develop without concomitant osteoarthritis. In this case, it may be a predictor of osteoarthritis. Several factors increase the likelihood of synovitis. The disease is prevalent in the knee joint with involvement of the suprapatellar pouch.
Synovitis is treated mainly by conservative methods. If the disease is chronic or proliferative, surgery may be indicated.
Types
According to etiology, two types of synovitis are distinguished:
- Idiopathic, when the cause cannot be determined;
- Secondary, which is caused by a background disease.
According to the activity of the pathological process, three forms are distinguished:
- a disease with minimal activity;
- moderate activity;
- a highly active disease.
According to the nature of the inflammatory process, the following forms are distinguished:
- exudative – characterized by an accumulation of inflammatory fluid in the joint cavity;
- proliferative, in which there is localized or diffuse overgrowth of the synovial membrane;
- adhesive – due to chronic inflammation, connective tissue strands begin to form.
Symptoms of synovitis
The lesion of a particular joint determines the clinical signs of synovitis. The leading symptom is pain, as a result of which the amplitude of movement is limited. The joint is swollen, red, and painful on palpation, and the skin is hot to the touch. Pain may be insignificant at the initial stage of the inflammatory process; as the disease progresses (in the absence of treatment), pain sensations become constant – moderate or severe.
The chronic course of the inflammatory process leads to a loss of elasticity in the ligamentous compartment. Because of this, the stabilizing function of the joint suffers, and the usual dislocations and subluxations may occur. During remission, the person may be bothered by mild pain and discomfort, and there is a periodic joint block.
In the case of bacterial lesions of the synovium, the disease has an acute course with vivid clinical symptoms. Inflammation is often purulent. The joint is significantly increased in volume due to edema, the pain is intense, and the skin is reddened and hot to the touch. The general body temperature is often elevated with a purulent process, and weakness and malaise are noted. Local lymph nodes react to the infection – they become enlarged and painful.
Causes of synovitis
Causes of synovitis may include the following:
- osteoarthritis – degeneration of articular cartilage and underlying bone that is accompanied by an inflammatory response;
- acute traumatic injuries to joint structures;
- chronic traumatism, including as a result of occupational hazards (construction workers, musicians, dentists, and other professions);
- metabolic disorders, in particular, purine metabolism disorders in gout;
- autoimmune dysfunction characteristic of rheumatoid arthritis, joint lesions in psoriasis;
- hemophilia is an X-linked blood clotting disorder that leads to bleeding, including periarticular hemorrhages;
- bacterial contamination, which can be the result of the spread of infection through blood or lymphatic flow or direct infection from open skin lesions;
Diagnosis of synovitis
Diagnosis of synovitis is based on clinical evaluation of existing complaints, anamnestic data, and objective examination results with the detection of signs of inflammation. Additional examination is required to confirm the diagnosis.
- Ultrasound scanning of joint and periarticular structures. Ultrasound can assess the condition of the soft tissue compartment and determine the presence of intra-articular fluid, the appearance of which indicates an inflammatory process.
- Arthrocentesis and cytologic analysis of the obtained fluid. In the presence of exudate, an increased number of leukocytes is determined. In the case of purulent inflammation, pathogenic bacteria can be detected.
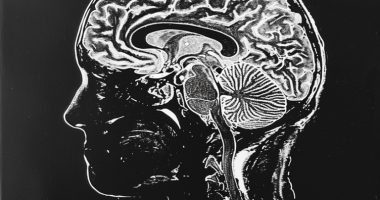
- Magnetic resonance imaging. Unlike computed tomography, this study allows a detailed assessment of the condition of tendons, joint capsules, synovial bags, and pockets. MRI may be required not only at the initial diagnosis stage but also for detailed surgery planning.
Bacterial infection in the general clinical blood test detects increased leukocytic cells, a relative increase in neutrophils, and accelerated erythrocyte sedimentation to the bottom of the tube. If autoimmune pathology is suspected, rheumatoid tests are particularly informative. In the case of gouty etiology, a biochemical blood test with an assessment of purine metabolism is indicated.
Histologic examination may be indicated in complicated clinical cases, including pigmented villous synovitis. Material for diagnosis is obtained by arthroscopy with biopsy. The study of the tissue structure of suspicious areas makes it possible to establish a definitive diagnosis and determine the program of further treatment.
Treatment of synovitis
In most cases, the therapeutic effect can be achieved with conservative treatment. In case of its ineffectiveness, in case of chronic forms, or case of purulent process, the question of surgery for synovitis is decided.
Conservative treatment
The mainstays of conservative treatment are:
- ensuring functional rest and immobility of the joint – orthoses, tight bandaging, walking on crutches, limitation of physical activity, and compliance with the home regime are used;
- local and systemic use of non-steroidal anti-inflammatory drugs that help to control pain syndrome;
- antibiotics – used in the bacterial form of the disease;
- local injection of hyaluronic acid into the affected joints.
Surgical treatment
The operation consists of partial excision of the synovial membrane in the affected areas. In some cases, total synovectomy is indicated.
The affected joint’s opening, sanitation, and drainage are indicated in purulent synovitis. At the same time, powerful antibacterial and anti-inflammatory therapy is carried out.
All these treatment options are available in more than 670 hospitals worldwide (https://doctor.global/results/diseases/synovitis). For example, diagnostic arthroscopy is performed in 15 clinics across Turkey for an approximate price of $2.4 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/diagnostic-arthroscopy).
Synovitis prevention
Prevention of synovitis includes adhering to the following recommendations:
- timely treatment of predisposing diseases;
- injury prevention;
- regular joint warm-ups in people with occupational hazards;
- exclusion of allergenic foods from the diet;
- optimizing physical activity.
Rehabilitation
After surgical intervention, joint development with physical therapy, massage, or physiotherapy is indicated.