Deep vein thrombosis (DVT)
What’s that?
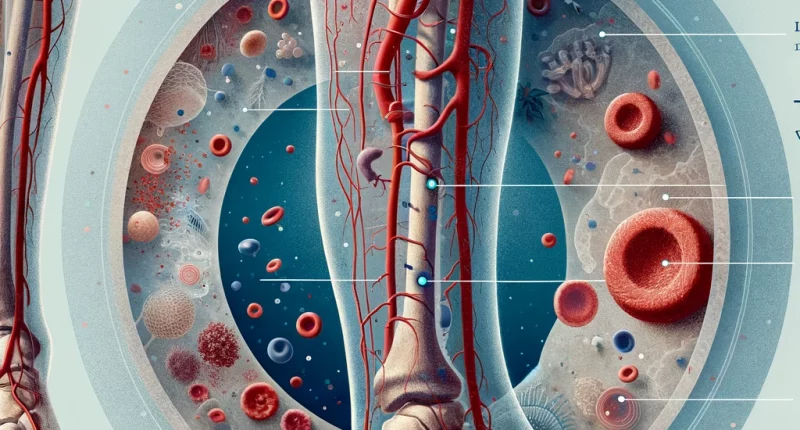
Venous thrombosis is an acute pathological condition where a blood clot blocks the vessel lumen. This pathology develops due to slow venous outflow, coagulation disorders, or damage to the venous walls.
Venous thrombosis is a common disease. It often develops as a complication of chronic venous insufficiency. Clinical manifestations are vivid – pain of a rasping character and pronounced limb swelling. The most dangerous variant of the disease is floating thrombosis. In this case, the blood clot can easily break off and migrate to other areas. It is fraught with thromboembolism of the pulmonary artery, the development of pulmonary infarction, and death. For patients with venous thrombosis, there is an increased risk of disability as a result of post-thrombotic syndrome (residual changes after the thrombosis itself has resolved).
Treatment is carried out in inpatient settings. Therapy is chosen based on clinical manifestations and laboratory and instrumental diagnostics results. Complex conservative treatment is possible. In acute disorders of blood flow, the clot is removed surgically.
Types of thrombosis
Based on the localization of the blood clot, thrombosis is distinguished:
- migratory;
- post-injection;
- of the superficial veins;
- deep veins.
Focusing on the relationship of the thrombus to the venous wall, thrombosis can be:
- occlusive;
- wall-to-wall;
- free-floating;
- mixed.
The clot may form in the inferior or superior vena cava system or in the sinuses of smaller vessels.
Symptoms of thrombosis
Thrombophlebitis of superficial veins is manifested by painful areas in the area of the clot and thickening of the vessel. Near the site of occlusion, hyperemia and edema quickly develop. When pressing the thrombosed vein with a finger, the patient feels pain.
A sudden pain in the limb, which increases with physical activity, may indicate a violation of deep vein patency. After a while, the areas below the thrombus swell, and the skin becomes bluish. Its surface becomes shiny. The patient complains of pain in the affected leg. Local hyperthermia is detected when touching – an increase in skin temperature in the occlusion area by 1.5-2°C. Approximately on the 2-3rd day, a network of dilated venous vessels with partial blood outflow is visible.
In some patients, thrombosis is asymptomatic because the blood drains through the communicating vessels. Deep vein occlusion may be indicated by a network of dilated veins on the abdomen or in the hip joints, thighs, and shins.
Causes of thrombosis
Blood clots are triggered by:
- damage to the inner vascular wall (as a result of infection, intoxication, autoimmune reactions, trauma);
- blood coagulation disorders;
- congestion.
Clots are formed at the confluence of these circumstances. For example, under conditions of increased blood viscosity, the trigger can be even a small injury to the endothelium, developing against the background of a cold. Violations of venous patency contribute to thrombus enlargement and more rapid development of inflammation of the venous wall. Occlusion of deep veins with thrombus more often develops against the background of inactive lifestyle, in combination with bad habits and chronic diseases. The provocateurs of thrombosis in the veins are:
- operations;
- trauma;
- childbirth;
- prolonged sitting;
- taking oral contraceptives in women at risk;
- oncologic pathology of abdominal organs;
- obesity;
- cardiovascular disease.
The risk of venous thrombosis is higher in older patients with diagnosed venous insufficiency. Patients who are forced to stay in bed for a long time due to the underlying disease or its treatment are also at risk.
Diagnosis of thrombosis
Diagnosis is often made by a phlebologist based on the data of anamnesis, laboratory, and instrumental examination methods. Following symptoms are specific for vein occlusion:
- Homans sign – bending the foot on the back side, the person feels pain in the calf muscle;
- Moses sign – soreness occurs when the tibia is compressed from front to back;
The doctor performs a tourniquet and marching test. The persistence of edema and severity of peripheral vessels indicate the presence of a thrombus. The tasks of further examination are:
- setting the localization and size of the clot;
- assessing the degree of circulatory collapse;
- to determine the type of clot;
- assessing the risk of pulmonary embolism;
- identifying the cause of thrombus formation.
Laboratory diagnostics include general and biochemical blood tests and urine examinations. An indirect sign of thrombosis is an increase in fibrin degradation products.
“The gold standard” of instrumental diagnostics is recognized as an ultrasound examination of blood flow with color mapping. The method allows you to detect a thrombus, its size, exact localization, and the state of the surrounding tissues. In some cases, when ultrasound is uninformative, CT or MRI with contrast is performed, and retrograde or ileocavography (invasive technique) is less often used.
Treatment methods
Thrombosis therapy aims to eliminate the thrombus, reduce the risk of vascular embolization, eliminate the causes of pathology, and restore normal blood circulation in the affected area. With non-embolized thrombi, conservative treatment is prescribed. If the risk of clot migration is high, surgery is performed.
Conservative treatment
Patients are shown a regimen that includes measured walking and special exercises to improve venous outflow. Elastic compression involves daily bandaging the entire lower leg to the middle or upper thigh. Drug treatment includes the use of:
- direct and indirect anticoagulants;
- hemorheological drugs;
- thrombolytics;
- diuretics;
- antiplatelet drugs;
- venotonics.
Antibiotic therapy is carried out in the hospital for thrombosis of septic origin.
Surgical treatment
If conservative treatment is not possible or the patient has a high risk of thrombus detachment, invasive treatment methods are used:
- Regional thrombolysis. Drugs are injected into the clot using a catheter, which helps it to dissolve.
- Placement of a cava filter. The device is implanted in the inferior vena cava to prevent pulmonary embolism in case of recurrent thrombosis.
- Crossectomy operation. It involves crossing the great saphenous vein and ligating its junction to stop the process of thrombus spreading.
- Radical thrombectomy. It involves removing the thrombus from the affected vein.
All these treatment options are available in more than 770 hospitals worldwide (https://doctor.global/results/diseases/deep-vein-thrombosis-dvt). For example, Inferior vena cava (IVC) filter placementcan be done in 8 clinics across Germany for an approximate price of $11.5 K (https://doctor.global/results/europe/germany/all-cities/all-specializations/procedures/inferior-vena-cava-ivc-filter-placement).
Prevention
To prevent venous thrombosis, excluding or minimizing the influence of risk factors is necessary. Normalization of weight and motor activity, timely treatment of acute diseases, and control of chronic diseases are required. Patients undergoing surgery are shown the maximum possible reduction of bed rest and early activation. In some cases, doctors prescribe drugs that prevent the formation of blood clots (antiplatelet drugs or anticoagulants).
Rehabilitation
After surgical treatment, the patient’s condition is monitored in the hospital for several days, and complex medication, elastic compression, and a dosed activity regimen are prescribed. After discharge, moderate exercise in the form of walking is allowed.