Hyperparathyroidism
Hyperparathyroidism is a condition of increased endocrine activity of the parathyroid glands.
About the disease
The parathyroid gland is a cluster of rounded cells located at the back of the thyroid gland, directly adjacent to it. In humans, there are most often 4 of these corpuscles (2 each on the side of the left and right lobe of the thyroid gland). These organs produce parathormone.
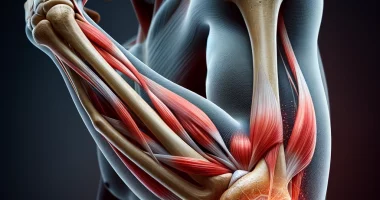
The regulation of parathyroid gland activity is based on the feedback principle. A decrease in calcium levels in the blood activates the production of parathormone. As a result, bone tissue is broken with the release of calcium into the bloodstream. At the same time, phosphorus excretion with urine increases, which is aimed at maintaining calcium-phosphorus balance.
The duration of its increase largely determines the biological effect of parathormone. Thus, with a single spike, on the contrary, bone formation is stimulated. If there is a prolonged increase in the concentration of the parent hormone, bone tissue is destroyed.
Most often, hyperparathyroidism occurs in patients in the 4th-5th decade of life. The risk group includes postmenopausal women and patients with urolithiasis. Elevated blood calcium levels are the predominant laboratory sign of the primary form of parathyroid hyperfunction. Repeated detection of this sign is an indication of the activity of parathormone. The primary method of topical diagnosis is scintigraphy of the parathyroid gland with technetium. Ultrasound is not always informative in the assessment of this condition.
The most common cause of hyperparathyroidism is a tumor of the parathyroid glands. Therefore, the basic method of treatment is considered to be surgical.
Classification of hyperparathyroidism
The etiologic classification of hyperparathyroidism involves distinguishing three major forms:
- primary – this is a pathological condition of the parathyroid gland, which leads to increased synthesis of parathormone and, therefore, manifests itself by an increase in calcium in the blood.
- secondary – compensatory activation of parathyroid glands in response to long-term decreased blood levels of calcium and increased phosphorus;
- tertiary is an autonomous synthesis of parathormone by parathyroid glands and the formation of secondary adenoma against the background of long-term compensatory activation.
Based on symptomatology, two forms are distinguished:
- clinical form – renal, bone, mixed (cardiovascular, gastrointestinal and other manifestations);
- subclinical variant.
Symptoms and signs of hyperparathyroidism
Symptoms of hyperparathyroidism are not specific, and the disease has been subclinical for a long time. Usually, the suspicion of this pathology appears at accidental detection of osteoporosis, gratuitous low-energy fractures, with changes in the level of calcium in the blood (increase or decrease), and urolithiasis.
In the development of persistent hyperparathyroidism, clinical manifestations are very diverse and depend on the premorbid background (concomitant diseases and conditions). Early clinical signs of hyperparathyroidism usually include diffuse osteoporosis. The presence of concrements in the kidneys or bladder is usually detected among the internal organs. Often, there is an associated pathology of the digestive system – ulcerative lesions of the stomach and duodenum. Such patients complain of dyspepsia – nausea, vomiting, belching, abdominal bloating, stool disturbance, etc.
High calcium levels contribute to high blood pressure, heart rhythm disorders, calcification of arterial walls and myocardium. Hypercalcemia can provoke neurological disorders.
Causes of hyperparathyroidism
The most common cause of primary hyperparathyroidism is a single parathyroid adenoma. Multiple tumors are much less common. Idiopathic hyperplasia of the parathyroid gland is also possible. In 1-5% of cases, epithelial cells have malignant degeneration.
Secondary hyperparathyroidism is more often associated with low blood levels of vitamin D or chronic kidney disease. Less often as a cause is found syndrome of impaired absorption, insufficient liver function, and use of pharmacological drugs that alter the metabolism of vitamin D in the body (corticosteroids, antimycotic drugs). Low blood calcium levels stimulate the parathyroid glands. Raising the level of parathormone should restore calcium-phosphorus metabolism in the body. However, if this situation continues for a long time, secondary hyperparathyroidism is transformed into tertiary.
Diagnosis of hyperparathyroidism
Laboratory diagnosis of hyperparathyroidism has certain features depending on the form of this condition.
- In the primary hyperfunction of parathyroid glands, an increase in calcium concentration, a decrease in plasma phosphate concentration, increased excretion of calcium with urine, a decrease in the relative value of tubule reabsorption of phosphates, an increase in alkaline phosphatase activity (characterizes the rate of bone destruction) in serum is detected.
- In secondary hyperparathyroidism, the calcium level in the blood is usually reduced. At the same time, the content of parathormone is elevated, which is an essential differential diagnostic sign.
The following methods are commonly used to determine the anatomical characterization of the parathyroid glands:
- ultrasound scans of the thyroid and parathyroid glands;
- bone ultrasound densitometry, which can detect even minimal decreases in bone mineral density;
- radioisotope methods (radionuclide scanning of parathyroid glands, scintigraphy);
- radiological methods (CT, MRI, positron emission tomography of the neck and mediastinum);
- X-ray bone scan (osteoporosis is detected if 20-30% of bone tissue is lost);
- X-ray bone densitometry is the most accurate method of determining bone density;
- selective arteriography.
Treatment of hyperparathyroidism
Treatment of hyperparathyroidism is carried out in all patients, even in the absence of clinical symptoms. Such a rule is dictated by the fact that against the background of this condition, there is an increased risk of sudden death. Depending on the form of the disease, conservative therapy or surgical intervention may be indicated.
Conservative treatment
Conservative therapy is carried out in secondary hyperparathyroidism. It aims to restore the level of vitamin D in the blood and treat diseases of the kidneys and digestive system.
Surgical treatment
When a tumor or hyperplasia of the parathyroid glands is verified, surgery is the only option for pathogenetic treatment. In the case of a single tumor, the affected gland is removed. In hyperplasia – partial excision with subsequent correction of postoperative hypoparathyroidism is indicated.
All these treatment options are available in more than 370 hospitals worldwide (https://doctor.global/results/diseases/hyperparathyroidism). For example, parathyroidectomy can be performed in 14 clinics across Turkey for an approximate price of $3.6 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/parathyroidectomy).
Prevention
To prevent secondary hyperparathyroidism, it is essential to control the level of vitamin D in the blood and timely treat diseases of the kidneys and digestive system.
Rehabilitation
Most often, primary hyperparathyroidism is sporadic. However, this pathology can have a genetic background (up to 10% of cases). Usually, in such cases, symptoms appear very early, and after surgical removal of the tumor, there is a high risk of recurrence and development of tumors in other organs. Therefore, such patients need regular monitoring by an endocrinologist throughout their lives.