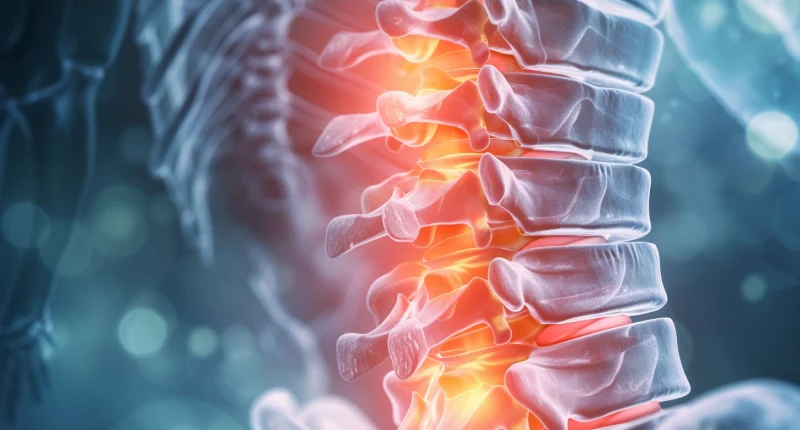
Spinal stenosis
What’s that?
Spinal canal stenosis is a pathological narrowing of the lumen, which can occur in the central, lateral zone, or in the area of the intervertebral foramen. The basis of the disease is the compression of nerve fibers by soft and bony tissues that penetrate the canal cavity.
Due to compression of the spinal cord or spinal nerves, a neurological deficit develops with a typical clinical picture. Most patients suffer from pain syndrome and sensory disturbances. The localization of discomfort sensations depends on the level of the spinal cord lesion. The disease develops in the lumbar spine in 80-90% of cases.
Spinal canal stenosis is a pathology that is characterized by a gradual nature of development. It contributes to the timely diagnosis of the disease with the subsequent selection of adequate treatment. In 85-90% of cases, unpleasant symptoms can be eliminated with the help of conservative therapy. Only if medication is ineffective a scheduled neurosurgical operation is prescribed.
Types of spinal canal stenosis
Spinal canal stenosis is a disease that can be congenital or acquired. In the first case, the cause of pathology is anomalies in the development of the spine, fusion of intervertebral discs, additional bone structures on their surface, and hypertrophy of the ligamentous apparatus that fixes the vertebrae. All these changes lead to the narrowing of the lumen of the spinal canal with the development of a characteristic clinical picture.
In most cases (up to 80%), the disease has an acquired (secondary) character. Pathology develops against the background of degenerative processes in the spine, which various reasons can cause.
Depending on the etiology, secondary spinal canal stenosis comes in:
- post-traumatic;
- post-operative;
- from an infectious process;
- the result of other degenerative spinal diseases (spondylosis, facet joints, scoliosis, lordosis).
Depending on the nature of the compression of nerve fibers, neurosurgeons distinguish central, lateral, and foraminal (in the area of the intervertebral foramen) spinal canal stenosis.
Symptoms of stenosis
Stenosis of the spinal canal is characterized by a lesion of fibers that pass inside and spread to the peripheral parts of the body. Compression of nerve pathways is accompanied by impairment of their function due to compression of micro-vessels, lymphatic pathways that supply these structures with nutrients. As a result, ischemia, edema, and demyelination develop, worsening the transmission of impulses along the affected fibers. Against the background of these changes, the patient presents the following complaints:
- Pain in the area of the affected part of the spine. Characteristic is the connection of the pain syndrome with the patient’s physical activity. Discomfort increases with movements accompanied by a narrowing of the intervertebral foramen (bending, walking downstairs, prolonged stay in an upright position).
- Sensory disturbance. The patient may complain of an inability to identify objects by touch and impaired perception of heat and cold by the skin.
- Muscle weakness, deterioration of motor skills, coordination of movements.
- Parasthesias.
The clinical picture directly depends on the localization of the maximum compression of the spinal canal. In 75-90% of cases, the disease develops in the lumbar region. It determines the patient’s predominant lesion of the lumbar, gluteal region, and lower extremities.
Pain, in this case, has a constant character. The severity of the symptom depends on the degree of nerve root and fiber compression. Patients note decreased discomfort when squatting, which increases with active walking or extension of the spine. Discomfort can spread to the posterior surface of the lower extremities, accompanied by a loss of patient stability.
Causes of stenosis
The pathogenetic basis for the development of the disease is the mechanical compression of nerve fibers that pass inside the spinal canal or at the sites of origin of spinal nerves.
The most common causes of pathology are:
- congenital abnormalities of the spine;
- traumatic injuries to the spinal canal, including surgery;
- infections with central and peripheral nervous system involvement;
- growth of osteophytes (bone outgrowths) against the background of osteoarthritis;
- scoliosis, lordosis;
- Bechterew’s disease;
- the formation of the facet joints;
- hypertrophy of the ligaments of the vertebral column;
- intervertebral disc pathology;
- spondylolysis and/or spondylolisthesis.
Stenosis of the intervertebral canal is a disease that develops gradually. In 90% of cases, the pathology results from another disease. However, some factors increase the risk of developing this problem:
- obesity;
- spinal injuries;
- heavy physical activity (weightlifters, movers);
- metabolic disorders (diabetes mellitus);
- menopause in women.
According to statistics, the disease develops in 1-2% of the world’s population. Predominantly, men, after 50 years of age, suffer from the disease.
Diagnosis of stenosis
Spinal canal stenosis is a pathology that the doctor can suspect even at the stage of the initial conversation with the patient. The neurosurgeon pays attention to characteristic pain in the lumbar back, discomfort in the legs, and other signs described above. Primary contact with medical personnel occurs more often at the district therapist or family doctor level. Having identified typical symptoms, these specialists refer the patient to a neurosurgeon.
In addition to collecting anamnesis and analyzing the patient’s complaints, the following methods are used in the diagnosis of the disease:
- Magnetic resonance imaging (MRI) of the spine. A mandatory procedure that allows for complete visualization of the spinal canal and identification of areas of nerve fiber compression.
- Review spondylography with functional tests in the anterior and lateral projection. This procedure is used to comprehensively assess the spinal column and its bony structures in dynamics.
The above methods are mandatory to establish the localization of the pathological process and assess the severity of the patient’s condition. To obtain more accurate information, the neurosurgeon may also prescribe:
- spinal ultrasound;
- multispiral computed tomography scan;
- intervertebral joint blockade;
- selective spinal cord blockade.
In parallel, the doctor prescribes a standard set of laboratory examination methods, which includes a general blood and urine analysis and biochemical analysis of blood.
Treatment methods
Treatment of spinal canal stenosis is always aimed at eliminating the compression of nerve fibers. Achieving this goal leads to the normalization of nutrition, blood, and lymph flow from the pathological area. It normalizes the patient’s condition, reduces or completely eliminates pain syndrome, and restores the affected limbs’ function.
Conservative treatment
In most cases, patients with spinal canal stenosis manage to achieve a stable remission with the help of medications. Doctors mainly use the following groups of drugs:
- Non-specific anti-inflammatory drugs (NSAIDs). These medications reduce pain and contribute to the inhibition of the local inflammatory process.
- Diuretics. The main task of this group of drugs is to reduce local edema.
- Myorelaxants. Used to improve muscle function and reduce spasms.
- Antibacterial and antiviral medicines. They are used only in the presence of a confirmed pathogen.
- B vitamins. These drugs improve the nervous system’s function, accelerating the recovery of damaged fibers.
Physiotherapy demonstrates promising results. With the help of ultrasound, magnetic field, and ultra-high frequency waves, it is possible to improve local microcirculation, reduce swelling, and stabilize the function of nerve endings.
Surgical treatment
If the conservative approach is ineffective, the neurosurgeon recommends surgery to the patient. In 95% of cases, such intervention is planned, which allows for full preparation of the patient and thus prevents the risks of developing any complications.
All surgical interventions for spinal canal stenosis have one goal – to reduce or eliminate compression of nerve endings. To accomplish this, a neurosurgeon may perform the following surgical options:
- resection of part of the arch of the superior and inferior vertebrae;
- removal of part of the base of the spinous process in the pathologic area;
- dilation of the intervertebral foramen;
- removal of the intervertebral joint.
The neurosurgeon sometimes combines these surgeries to achieve an optimal result. The choice of technique is always made individually, depending on the peculiarities of a particular clinical case, its severity, and the localization of the stenosis.
All these treatment options are available in more than 800 hospitals worldwide (https://doctor.global/results/diseases/spinal-stenosis). For example, foraminotomy can be done in 31 clinics across Turkey for an approximate price of $4.8 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/foraminotomy).
Prevention
There is no specific prevention of spinal canal stenosis. The patient is left to work with risk factors, which include:
- weight control;
- timely treatment of spinal disorders;
- moderate physical activity;
- avoiding traumatic injury;
- regular check-ups with your doctor.
If the first signs of the disease are detected, specialized help should be sought as early as possible.
Rehabilitation
Recovery after surgical treatment of spinal canal stenosis takes place in inpatient and outpatient settings. For the first few days, the patient remains under the supervision of a neurosurgeon who performs daily dressings and assesses the postoperative wound’s healing quality. After discharge, the patient gradually returns to a normal lifestyle.
Sutures are removed on the 7th-10th day. Complete recovery occurs within 1-6 months, depending on the age of the disease and the extent of surgical intervention. During this time, limiting physical activity and stress factors is recommended. It is necessary to eat a complete diet, rest, and follow the recommendations of the neurosurgeon.