Aortic valve stenosis
Definition
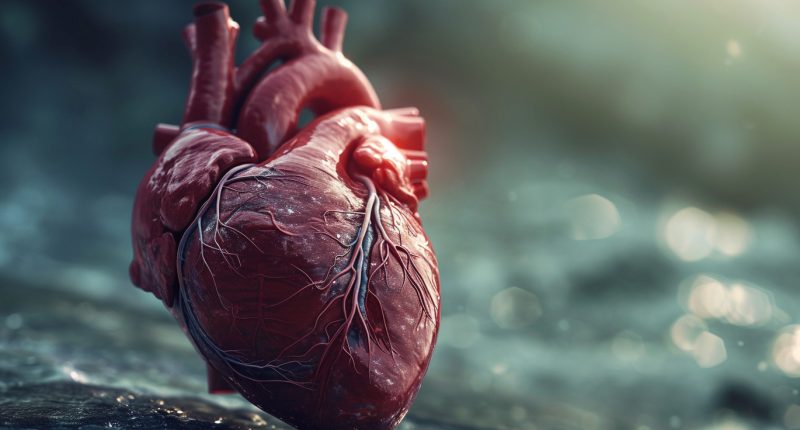
Aortic stenosis (AS) – is one of the most common heart defects. In this disease, the first part of the largest artery in the human body narrows. The pathological process affects the semilunar valve connecting the left ventricle to the aorta. In its normal state, it uses three valves to block the return flow of blood from the aorta to the ventricular cavity during diastole (relaxation of the heart muscle between contractions). Abnormal narrowing of the semilunar valve prevents blood flow to the heart’s other organs, and they do not receive enough oxygen and nutrients.
With aortic stenosis, there is a significant difference in pressure between the aortic and ventricular cavities, and the load on the heart muscle increases in all parts. Over time, the patient develops a severe hemodynamic disturbance. In men, the pathology is diagnosed 3-4 times more often than in women. Aortic stenosis is one of the most common acquired heart defects.
Types of aortic stenosis
Firstly, the disease is classified according to the origin of the disease:
- congenital (primary), which occurs as an independent disease.
- acquired (secondary) developing against a background of other diseases.
According to localization, aortic stenosis is divided into 3 types:
- valve defects, the most common, are diagnosed in 60% of cases.
- supravalvular, occurs in 6-10% of patients;
- subvalvular, found in 25-30% of cases.
Aortic valve stenosis degrees must be classified considering the pressure gradient. This term refers to the difference in blood pressure between the left ventricle before and after the semilunar valve. The stronger the contraction, the more the pressure increases.
The classification of the slope includes 4 degrees of aortic valve stenosis:
- mild stenosis, the valve opening is more than 1,2 cm2 pressure gradient of 10-35 mm Hg.
- moderate stenosis, mouth area 1.2-0.75 cm2, slope 36-65 mm Hg.
- severe stenosis, valve opening of less than 0.74 cm2, and a gradient of more than 65 mmHg.
- critical stenosis, the orifice is narrowed to 0.5-0.7 cm2, and the slope is above 80 mmHg.
The pathological process is divided into several stages, depending on the severity of the circulatory disorders.
- Amount of compensation. Mild degree of aortic stenosis. A valvular defect can be detected by auscultation of the heart. Myocardial functions are almost unchanged.
- Latent heart failure. Abnormalities are detected on chest X-ray and ECG. At this stage patients have their first complaints about deterioration in their health.
- Relative heart failure. No significant pathological changes appear at the junction of the semilunar valve and the left ventricle. The condition of patients deteriorates, and the list of complaints is increasing.
- Severe heart failure. The general condition of patients significantly worsens; there are specific complaints and severe disturbances in the heart and respiratory system work.
- Terminal. Severe degree of heart failure, in most cases leading to death.
Symptoms of aortic stenosis
In the early stages of the disease patients do not feel severe discomfort for long. The first signs of aortic stenosis appear when the aorta is narrowing by about 30%. At this time, the heart stops compensating for the valvular defect with increased work, and the person begins to feel:
- muscle weakness.
- rapid fatigue;
- shortness of breath during physical exertion;
- gratuitous palpitations.
Because of these symptoms, it is difficult to suspect the development of cardiac pathology, so many people are in no hurry to visit a cardiologist. As the disease progresses, specific signs of heart damage appear:
- heart rhythm disorders;
- irregular heartbeat;
- angina pectoris – periodic pressure, squeezing or pulling on the back of the sternum;
- shortness of breath during exercise, after exercise, and even at rest.
These signs are complemented by non-specific symptoms:
- pronounced swelling;
- frequent dizziness and headaches.
- weakness, rapid fatigue;
- periodic loss of consciousness.
The clinical picture may vary in the presence of concurrent heart disease or disease in other organs.
Causes of aortic valve stenosis
- Congenital heart defects
Congenital aortic valve stenosis is often associated with malformations like bicuspid aortic valve or congenital narrowing of the aortic orifice. Typically ,congenital valve stenosis affects patients under the age of 30, while acquired ones occur after 60.
- Rheumatic fever
Acquired pathological narrowing of the aortic orifice most often occurs as a complication of poorly treated strep throat.The damaged valve flaps become dense, rigid, and fuse.
- Aortic valve calcification
Calcium deposits can accumulate on heart valves causing stiffening, especially in individuals with congenital aortic valve defects. Symptoms of aortic valve stenosis related to age and calcium buildup typically appear around age 70 or 80.
Risk factors of aortic valve stenosis
Negative factors that accelerate the formation of aortic stenosis include:
- smoking
- hypertension
- hypercholesterolemia
- age-related calcification of the valve
- сhronic kidney disease
- aortic atherosclerosis
- infectious endocarditis
- systemic lupus erythematosus.
Diagnosis of aortic stenosis
First, the cardiologist will take a medical history, listen to the patient’s complaints, and perform a physical exam. Diagnostic measures to detect this pathology include:
- ECG shows left atrial and ventricular enlargement, blockage, and arrhythmia.
- chest X-ray reveals left ventricular enlargement, calcification of the valve orifice, enlargement of the aorta above valve;
- Echocardiography demonstrates calcified and thickened aortic valve leaflets, a hypertrophied left ventricle, and a reduced aortic valve orifice.
- Cardiac catheterization, an invasive diagnostic technique may also be used to help clarify the diagnosis; on its basis, the specialist can detect a decreased stroke volume and a change in the pressure ratio.
Laboratory tests for blood and urine tests are of an auxiliary nature.
Living with Aortic Valve Stenosis
Individuals with aortic valve stenosis can lead active lives with appropriate treatment and lifestyle adjustments. Education about the condition, adherence to treatment plans, and consistent medical follow-ups are vital.
Treatment of aortic valve stenosis
The choice of treatment strategy is determined by the degree stenosis and the severity of the symptoms. The main treatment strategies for aortic stenosis are medical therapy and surgery.
Conservative treatment
The treatment is ineffective. No drugs can stop the narrowing of the heart valve and restore the cavity opening. Conservative treatment is performed to relieve symptoms. The patient may be prescribed certain medications that can:
- control the heart rhythm;
- lower blood pressure;
- stop the pain behind the sternum.
This type of treatment is carried out both before and after surgery.
Surgical treatment
It is the most effective way to get rid of a patient’s cardiological problem. Several different interventions are used to eliminate valve failure.
- Aortic balloon valvuloplasty. A special balloon is inserted into it to enlarge the orifice of the aorta.
- Valve repair. For severe stenosis, dissection to change the structural elements of the valve is performed.
- Open heart valve replacement. A new valve is implanted in the patient. It can be either biological or mechanical.
- Transcatheter aortic valve replacement (TAVR): A minimally invasive procedure ideal for patients at high surgical risk, where a new valve is inserted via a catheter through a large artery.
All of these procedures are performed in more than 650 hospitals around the world. (https://doctor.global/results/diseases/aortic-valve-stenosis). For example, aortic valve replacement can be done in 29 clinics in Turkey for approximate $8.4 K. (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/aortic-valve-replacement-avr)
Prevention
Preventive measures are limited to preventing the development of diseases and pathological conditions that can cause aortic stenosis. People who are found to have initial changes in the aortic valve and those at risk and should be seen regularly by a cardiologist and rheumatologist.
Rehabilitation
Patients stay in the hospital for the first week after the operation. They will be monitored there around the clock by specialists. After discharge, the doctor will give a list of nutrition, exercise, and lifestyle recommendations. These must be done strictly. Also, during recovery, you must regularly visit your cardiologist and undergo an examination.
Advances in Aortic Valve Stenosis Treatment
Recent advancements in valve replacement techniques, particularly TAVR, have significantly improved outcomes for patients unsuitable for open-heart surgery. Ongoing research is focused on developing better prosthetic valves and less invasive treatment approaches.
Conclusion
Aortic valve stenosis is a serious heart condition that requires timely diagnosis and intervention to prevent severe complications. With advancements in diagnostic techniques and treatment modalities, including innovative surgical interventions, individuals with this condition can enjoy improved quality of life and longevity. Continued research and patient education are key to further advancements in the management and treatment of aortic valve stenosis.