Benign adrenal tumor
Definition
Benign adrenal tumors are focal overgrowths of adrenal cells. They may originate from the cortical or cerebral layers and have different histologic and morphologic structures and clinical manifestations. More often, they manifest themselves in paroxysmal manner in the form of adrenal crises: muscle tremors, increased BP, tachycardia, agitation, fear of death, abdominal and chest pain, and copious urine output. Treatment is always operative.
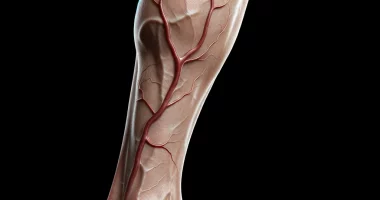
Anatomy
Adrenal glands are complex in histological structure and hormonal function. These endocrine glands are formed by two morphologically and embryologically different layers: external, cortical, and internal, cerebral.
The adrenal cortex synthesizes various steroid hormones:
- Mineralocorticoids involved in water and salt metabolism;
- Glucocorticoids involved in protein-carbohydrate metabolism;
- Sex hormones that cause the development of female or male secondary sex characteristics (estrogens, androgens, and progesterone in small amounts).
The inner medullar layer of the adrenal glands produces catecholamines: dopamine, norepinephrine, and adrenaline. These neurotransmitters transmit nerve impulses and affect metabolic processes. In the development of adrenal tumors, endocrine pathology is determined by the lesion of a particular gland layer and the specific action of the excessively secreted hormone.
Classification
By localization, adrenal neoplasms are divided into two large groups, fundamentally different from each other: tumors of the adrenal cortex and tumors of the adrenal medulla. Tumors of the outer cortical layer of the adrenal gland – aldosteroma, corticosteroma, androstroma and mixed forms – are rare. From the inner medullary layer of the adrenal gland come tumors of chromaffin or nerve tissue: pheochromocytoma (develops more often) and ganglioneuroma. Adrenal tumors originating from the medullary and cortical layers may be benign or malignant.
Benign adrenal neoplasms are usually small, without significant clinical manifestations, and are incidental findings on examination. In addition, primary adrenal tumors may be hormonally inactive (incidentalomas or “clinically silent” tumors) or produce an excess of some adrenal hormone, i.e., hormonally active.
- Hormonally inactive adrenal neoplasms are more often benign (lipoma, fibroma, myoma), with equal frequency developing in women and men of any age group, and usually accompany the course of obesity, hypertension, and diabetes mellitus.
- Hormonally active tumors of the cortical layer of the adrenal gland are aldosteroma, androsteroma, and corticosteroma; of the cerebral layer, pheochromocytoma. According to the pathophysiological criterion, adrenal tumors are subdivided into:
- that cause disorders of water-salt metabolism – aldosteromas;
- that cause metabolic disorders – corticosteromas;
- neoplasms that have a masculinizing effect – androsteromas;
- neoplasms that have a feminizing effect – corticoestromas;
Hormone-secreting tumors of the adrenal gland are of greatest clinical significance.
Symptoms of adrenal tumors
Adrenal tumors without hyperaldosteronism, hypercorticism, or autonomic crises are asymptomatic. As a rule, they are detected incidentally during MRI, CT, or ultrasound of the abdominal cavity and retroperitoneal space performed for other diseases.
Aldosteroma
An aldosterone-producing tumor of the adrenal gland originating from the tubular zone of the cortex and causing the development of primary aldosteronism (Conn’s syndrome). Aldosterone regulates the body’s mineral and salt metabolism. Excess aldosterone causes hypertension, muscle weakness, alkalosis (alkalinization of blood and tissues), andhypokalemia. Aldosteromas can be solitary (70-90% of cases) and multiple (10-15%), uni- or bilateral. An asymptomatic course of aldosteroma occurs in 6-10% of patients with this type of adrenal tumor.
Corticosteroma
Glucosteroma or corticosteroma is a glucocorticoid-producing tumor of the adrenal gland originating from the bundle zone of the cortex and causing the development of Icenko-Cushing’s syndrome (obesity, arterial hypertension, early puberty in children and early sexual decline in adults). Corticosteromas are the most common tumors of the adrenal cortex.
The clinic of corticosteroma corresponds to the manifestations of hypercorticism (Icenko-Cushing syndrome). Cushingoid-type obesity, hypertension, headache, increased muscle weakness and fatigue, steroid diabetes, and sexual dysfunction develop. The abdomen, mammary glands, and inner thighs show striae and petechial hemorrhages.
Pheochromocytoma
Catecholamine-producing tumors of the adrenal gland originate from chromaffin cells of the adrenal medulla (in 90%) or the neuroendocrine system (sympathetic plexuses and ganglia, solar plexus, etc.) and are accompanied by autonomic crises. Morphologically, pheochromocytoma more often has a benign course; its malignancy is observed in 10% of patients, usually with extra-adrenal localization of the tumor. Pheochromocytoma is more common in women between 30 and 50 years of age. 10% of this type of adrenal tumor is familial.
Complications
Among the complications of benign adrenal tumors, malignization is common. Malignant adrenal tumors metastasize to the lungs, liver, and bones. In severe course, pheochromocytoma crisis is complicated by catecholamine shock – uncontrolled hemodynamics, random change of high and low BP indices, and not amenable to conservative therapy. Catecholamine shock develops in 10% of cases, more often in pediatric patients.
Diagnosis
Modern endocrinology has diagnostic methods that allow the diagnosis of adrenal tumors and establish their type and localization. The functional activity of adrenal tumors is determined by the content of aldosterone, free cortisol, and catecholamines in daily urine.
In suspected pheochromocytoma and BP crises, urine and blood for catecholamines are collected immediately after or during the attack. Specific tests for adrenal tumors include taking blood for hormones before and after medication (captopril test, etc.) or measuring BP before and after medication (clonidine, and tyramine tests).
The hormonal activity of an adrenal tumor can be assessed using selective adrenal phlebography, which involves X-ray contrast catheterization of adrenal veins with subsequent blood sampling and determination of hormone levels. The study is contraindicated in pheochromocytoma because it can provoke the development of a crisis. The adrenal tumor’s size and localization and distant metastases’ presence are assessed by ultrasound of the adrenal glands, CT, or MRI. These diagnostic methods allow detection of tumors-incidentalomas with a diameter of 0.5 to 6 cm.
Treatment of adrenal tumors
Hormonally active adrenal tumors, as well as neoplasms with a diameter of more than 3 cm that do not show functional activity and tumors with signs of malignization, are treated surgically. In other cases, dynamic control of adrenal tumor development is possible. Operations on adrenal tumors are performed from open or laparoscopic access. The entire affected adrenal gland is removed, and in case of a malignant tumor, the adrenal gland and nearby lymph nodes.
Surgery for pheochromocytoma is the most difficult because of the high probability of severe hemodynamic disturbances. In these cases, great attention is paid to the preoperative preparation of the patient and the choice of anesthesia aimed at controlling pheochromocytoma crises. Pheochromocytomas are also treated with intravenous injection of a radioactive isotope, which causes a reduction in the size of the adrenal tumor and existing metastases.
Treatment of some types of adrenal tumors responds well to chemotherapy (mitotane). Suppression of pheochromocytoma crisis is carried out by intravenous infusion of phentolamine, nitroglycerin, and sodium nitroprusside. If it is impossible to control the crisis and the development of catecholamine shock, emergency surgery is indicated for vital indications. After surgical removal of the tumor together with the adrenal gland, the endocrinologist prescribes permanent replacement therapy with adrenal hormones.
All these treatment options are available in more than 580 hospitals worldwide (https://doctor.global/results/diseases/benign-adrenal-tumor). For example, Adrenalectomy can be performed in 17 clinics across Turkey for an approximate price of $7.2 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/adrenalectomy).
Prognosis
The timely removal of benign adrenal tumors accompanies a favorable prognosis for life. However, after the androsteroma is removed, patients often remain stunted. Half of the patients who underwent surgery for pheochromocytoma still have moderate tachycardia and hypertension (constant or transient), which is amenable to drug correction. When aldosteroma is removed, blood pressure returns to normal in 70% of patients. In 30% of cases, moderate hypertension persists, responding well to hypotensive therapy.
After benign corticosteroma is removed, symptoms are noted to recede in 1.5-2 months: the patient’s appearance changes, BP and metabolic processes become normal, pale striae normalize sexual function, manifestations of steroidal diabetes mellitus disappear, body weight decreases, and hirsutism decreases and disappears.
Prevention
Since the causes of adrenal tumor development are not fully established, prevention is limited to the prevention of recurrence of removed tumors and possible complications. After adrenalectomy, it is necessary to check patients with an endocrinologist once every six months with subsequent correction of therapy depending on the well-being and the results of tests.
Patients after adrenalectomy for adrenal tumors are contraindicated for physical and mental exertion, use of sleeping pills, and alcohol.