Cervical cancer
What is cervical cancer?
Cervical cancer is an oncological pathology of the female reproductive system characterized by malignant degeneration of epithelial cells of the cervical canal. According to statistics, this disease affects about 20 women per 100 thousand; the mortality rate is 9 cases per 100 thousand of the female population. Almost a third of patients come to the doctor with advanced stages of cancer. With timely diagnosis and treatment, it is possible to achieve full recovery.
Understanding Cervical Cancer
The transition from a normal cervical cell to a cancerous one is typically slow, often taking years but sometimes decades, which provides a significant window for detection and intervention. The infection with HPV is the most significant risk factor, but not all HPV infections lead to cervical cancer. The body’s immune system usually eliminates the virus before it causes harm. However, in a small percentage of women, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
Cervical cancer develops in several stages:
- Epithelial cell dysplasia (a precancerous condition).
- Malignant cellular degeneration with progression to non-invasive intraepithelial cancer.
- Microinvasive stage (no symptoms, surrounding tissues are affected, cells may penetrate the lymph stream).
- Clinical stage (symptoms appear, other internal organs are affected, metastases form).
Cervical cancer progresses slowly. A long dysplastic process precedes pathology. Timely preventive visits to the gynecologist can diagnose the disease at the earliest stages when it is possible to minimize traumatic treatment and complete patient recovery. The leading cause of mortality from cervical cancer is neglect of preventive visits to a specialist.
Symptoms of cervical cancer
The first stages of cervical cancer are usually asymptomatic. Clinical symptoms indicate the increase and spread of the malignant process, affecting internal organs and the lymphatic system. Common signs of cervical cancer are:
- heavy periods;
- intermenstrual bleeding;
- Contact bleeding (after sexual intercourse, physical exercise, gynecological examination);
- postmenopausal bleeding;
- copious vaginal discharge;
- pelvic pain.
In advanced cases, when the tumor decays, there may be a stinky discharge with pink color.” If the tumor infiltrates the rectum or bladder, fistulas may form, and feces may enter the vagina.
Causes of cervical cancer
Human papillomavirus is recognized as the leading cause of cervical cancer. Serotypes with high oncogenic risk (16, 18) are found in almost 90% of patients diagnosed with cervical cancer. The probability of getting sick increases in the presence of provoking factors:
- smoking;
- STD;
- chronic inflammatory diseases of the reproductive organs;
- cervical erosion;
- early onset of sexual activity;
- abortions;
- a history of multiple births;
- irrational diet;
- deficiency of vitamins A and C in the body;
- Age over 40.
In the group of increased risk are women whose close relatives have faced this disease. An additional predisposing factor is immune abnormalities.
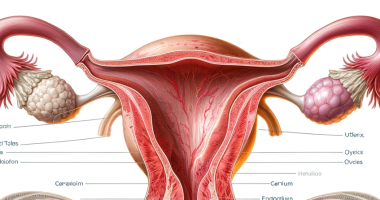
Diagnosis of cervical cancer
The basis of cancer prevention is regular checkups with a gynecologist, with cytologic examination of cervical smears. That makes it possible to diagnose cancer even at pre-invasive stages. During the examination, the doctor examines the cervix in mirrors and conducts instant tests (iodine and vinegar tests).
Invasive stages of cancer can be detected purely by visual inspection (by specific “growths” on the cervix, bumpiness, change in its shape, characteristic vascular pattern, bleeding of tissues at a light touch).
If cervical cancer is suspected, it is necessary to take a test for the SCC (squamous cell carcinoma) antigen (normal is lessthan 1.5 ng/mL). To confirm the diagnosis, a targeted biopsy or knife biopsy with scraping of the cervical canal is performed. The depth of tumor penetration is determined during cervical conization (taking a cone-shaped tissue fragment).
The results of histology are the primary criterion for diagnosis. To comprehensively diagnose the state of the patient’s body, general clinical tests are prescribed, and ultrasound of the pelvic organs, abdominal cavity, fluorography, cystoscopy, and other studies are performed.
Cervical cancer treatment
The primary treatment for cervical cancer is surgery. Depending on the type and stage of tumor development, as well as the age, health status, and reproductive plans of the woman, radical or organ-preserving intervention is performed. Surgical treatment is often combined with chemotherapy and/or radiation therapy.
Organ-preserving treatment tactics may be acceptable for young women with preinvasive cervical cancer who plan to give birth in the future. In case of widespread changes, the uterus, appendages, surrounding tissue, upper third of the vagina, and regional lymph nodes are removed, which helps to avoid recurrence. In the future, the patient will require complex rehabilitation.
All these treatment options are available in more than 900 hospitals worldwide (https://doctor.global/results/diseases/cervical-cancer). For example, total laparoscopic hysterectomy (TLH) can be performed in 32 clinics across Germany for an approximate price of $13.9 K(https://doctor.global/results/europe/germany/all-cities/all-specializations/procedures/total-laparoscopic-hysterectomy-tlh).
Recovery and Rehabilitation
Recovery and rehabilitation from cervical cancer treatment are highly individualized, depending on the extent of the disease and the treatment modality used. Surgical treatments can lead to physical challenges, which might require physical therapy, while radiation and chemotherapy can have side effects such as fatigue, which might be managed with dietary adjustments and exercise. Emotional and psychological support through counseling or support groups is also an integral part of recovery, addressing the impact of cancer diagnosis and treatment on mental health and quality of life.
Recovery varies based on treatment type and individual factors. Rehabilitation may involve physical therapy, nutritional support, and counseling to manage the physical and emotional impacts of cancer and its treatment.
Living with Cervical Cancer
Living with cervical cancer requires ongoing care and monitoring to manage symptoms, detect recurrence early, and address the psychological and social impacts of the disease.
Conclusion
Advancements in screening and HPV vaccination have significantly reduced the incidence of cervical cancer. Early detection and comprehensive treatment can lead to favorable outcomes, highlighting the importance of regular cervical health screenings and HPV awareness.