Chylothorax
Definition
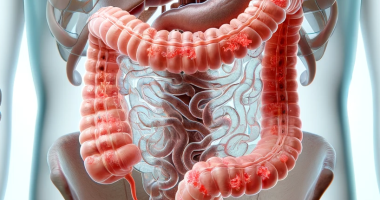
Chylothorax is a pathologic accumulation of lymphatic (chylous) fluid in the pleural cavity due to lymphorrhea from the thoracic duct. The development of chylothorax is accompanied by dyspnea, progressive deterioration of well-being, exhaustion, and respiratory failure. Chylothorax is diagnosed by clinical and anamnestic data, radiography, thoracocentesis, cytologic evaluation of chylous fluid, and thoracoscopy. Treatment of chylothorax includes repeated punctures or drainage of the pleural cavity to remove chylus, and in case of persistent lymphorrhea – ligation of the thoracic lymphatic duct, pleuroperitoneal shunt, pleurodesis, lymphovenous anastomosis, etc.
General information
Chylothorax is a relatively rare pathology that develops due to disruption of the thoracic lymphatic duct integrity and inflow of lymphatic (chylous) fluid circulating through it into the pleural cavity. Chylothorax may be accompanied by significant lymphorrhea (lymphatic effusion) – up to 4-5 liters per day and lead to profound respiratory, metabolic, and immunological disorders in the body, posing a threat to the patient’s life due to the loss of fats, proteins, vitamins, electrolytes, lymphocytes.
Chylothorax occurs in all age groups, including newborns. In clinical practice, specialists in thoracic surgery, traumatology, cardiac surgery, gastroenterology, oncology, pulmonology, phlebology, and lymphology encounter chylothorax.
Reasons
Chylothorax is a secondary disease or complication associated with the pathology of lymphatic vessels. Depending on etiologic factors, the following types of chylothorax are distinguished: congenital, traumatic, and nontraumatic. Also distinguish idiopathic chylothorax, which develops in smokers with many years of experience. Possible causes:
- Congenital pathologies. Chylothorax manifested during newborn and childhood may be due to hereditary atresia of the thoracic lymphatic duct and the presence of a fistula between its lower segment and the pleural cavity. In primary persistent fetal chylothorax, it is not always possible to identify the apparent cause of the disease (in rare cases, it may be hereditary lymphangiectasia).
- Iatrogenic injuries. Iatrogenic chylothorax develops mechanical damage of the thoracic lymphatic duct or its main branches during surgical interventions (thoracic, cardiosurgical, abdominal, spinal), diagnostic procedures (translumbar arteriography, catheterization of subclavian vein or left heart, esophagoscopy)
- Trauma. Traumatic chylothorax is the result of blunt trauma or penetrating injury to the thorax and neck. When the thoracic lymphatic duct is damaged above the level of V-VI thoracic vertebrae, left-sided chylothorax is formed, and below – right-sided. Idiopathic chylothorax is based on spontaneous rupture of the lymphatic vessel wall during coughing and pressure increase in the supradiaphragmatic region.
- Tumors. Chylothorax of nontraumatic genesis often occurs in the presence of various benign and malignant neoplasms affecting the lymphatic system of the mediastinum and neck (mediastinal malignant non-Hodgkin’s lymphoma, benign ductal lymphangioma, mediastinal lymphangiomatosis, pleural cancer).
- Diseases of the thoracic and abdominal cavity organs. Intrathoracic tuberculosis and sarcoidosis, mediastinitis, ascending lymphangitis, amyloidosis, diaphragmatic hernia, etc., can lead to the development of chylothorax. Accumulation of chyle fluid in the pleural cavity can be noted in superior vena cava syndrome, accompanied by increased venous pressure and hypertension in the thoracic lymphatic duct system. Pseudochylothorax develops due to the chronization of pleural effusion (in tuberculosis and rheumatoid arthritis). Pseudochylous exudate has a turbid milky-white color, peculiar opalescent sheen, and high cholesterol content.
Pathogenesis
Chyle fluid has a whitish color and contains a large number of chylomicrons, which are the main transport form of triglycerides, cholesterol, and exogenous fatty acids. Chylomicrons are formed in the epithelial cells of the intestinal mucosa; after absorption through the lymphatic pathways, they enter the thoracic lymphatic duct and further into the circulatory system. In chylothorax, in addition to high lipid content (more than 1.1 mmol/L), in pleural chyle exudate, there is an excess of the total number of cellular elements (more than 1000 per μL) and lymphocytes (more than 90%).
Symptoms of chylothorax
Postoperative chylous pleurisy is characterized by gradual development. This is due to the gentle diet during the rehabilitation period, the insignificant amount of lymph, and its slow penetration into the pleural cavity. Therefore, postoperative chylothorax is usually recognized only 2-10 days after surgical intervention. Clinical manifestations occur when the volume of chylous effusion reaches 200 ml or more.
The first sign is dyspnea, which may progress to respiratory failure as chylothorax increases. There is heaviness in the corresponding half of the chest, tachycardia, hypotension, and development of a collapsed state. Unlike exudative pleurisy, chest pain and hyperthermia are atypical for chylothorax because lymph does not irritate the pleura and, due to its bacteriostatic properties, is able to stay uninfected for a long time.
Critical is lymphorrhea up to 1.5-2 liters per day, as a significant amount of protein, fats, electrolytes, and lymphocytes are lost along with lymph. Prolonged or massive loss of lymph causes the development of metabolic disorders, immunodeficiency, and exhaustion of the patient, which can lead to death.
Diagnosis
Physical findings in chylothorax resemble the signs of pleurisy. There is a dulling of percussion sound and a weakening of breathing on the side corresponding to the lesion. Physical examination data are clarified with the help of instrumental diagnostics:
- Radiologic methods. Lung radiography determines the presence of effusion in the pleural cavity, lung compression, and displacement of the mediastinum. To clarify the causes of chylothorax, ultrasound examination of lymphatic vessels, lymphangiography, lymphoscintigraphy, and chest CT are necessary.
- Diagnostic pleural puncture. It is performed based on the radiological picture and ultrasound data of the pleural cavity. In chylothorax, chyle fluid of a milky-white color is obtained. Analysis of pleural effusion reveals the oily character of the exudate, the high content of lymphocytes, triglycerides, and the total number of cellular elements typical for lymph.
- Blood tests. In chylothorax, lymphopenia and hypoproteinemia increase in the blood.
- Invasive diagnosis. To determine the exact cause of nontraumatic chylothorax, biopsy of the lymph node, pleura, and lung tissue, diagnostic thoracoscopy or thoracotomy, and morphologic examination of biopsy material may be required.
Treatment of chylothorax
Conservative tactics
Treatment is started with conservative methods: they help to achieve spontaneous cessation of lymphorrhea in almost 50% of patients with asymptomatic or asymptomatic chylothorax. In conservative management of chylothorax, the pleural cavity is drained with a permanent drain or a series of pleural punctures with evacuation of chylous fluid. This achieves decompression of the lung and mediastinal organs and reduction of respiratory disorders.
To reduce chylous production, the patient is completely transferred to parenteral nutrition, or a high-calorie diet with fat restriction is prescribed. Infusion therapy with protein and salt preparations is carried out to correct hypoproteinemia and electrolyte disorders in chylothorax. Intravenous administration of somatostatin is successfully used to resorb effusion.
Surgical treatment
If conservative measures are unsuccessful and lymphorrhea persists, it is advisable to switch to surgical tactics. The main types of operations performed in chylothorax are:
- pleuroperitoneal shunt;
- ligation of the thoracic lymphatic duct above and below the fistula;
- obliteration of the pleural cavity with talc (pleurodesis);
- lymphovenous anastomosis.
Successful cases of lymphatic duct embolization in adult patients have been described. Specific treatment is indicated for chylothorax caused by tuberculosis, and chemoradiation therapy is indicated for tumor etiology.
All these treatment options are available in more than 530 hospitals worldwide (https://doctor.global/results/diseases/chylothorax). For example, Diagnostic thoracoscopy can be done in 27 clinics across Turkey for an approximate price of $3.3 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/diagnostic-thoracoscopy ).
Prognosis and prevention
Chylothorax’s lethality ranges from 15 to 50%. It has a prognostically unfavorable course in malignant neoplasms of the thoracic cavity. However, with timely diagnosis and complex treatment of traumatic chylothorax, positive results can be achieved in most cases.
Prevention of iatrogenic chylothorax consists of careful and justified diagnostic manipulations, invasive therapeutic procedures, and surgical interventions. In thoracic trauma, it is always necessary to remember the possibility of damage to the thoracic lymphatic duct and the development of chylothorax. Prevention of idiopathic chylothorax dictates the need to stop smoking.