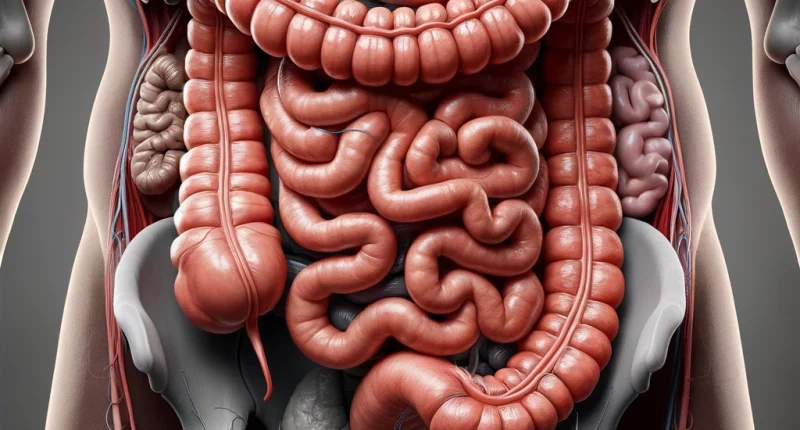
Colon polyps
Overview
Colon polyps are tissue formations that grow from the intestinal mucosa into the colon lumen. As a rule, they are asymptomatic, sometimes manifesting themselves with stool disturbance and blood in it, as well as abdominal pain. The danger of these neoplasms lies in the risk of their transformation into a malignant tumor – colon cancer. Preventing complications involves monitoring your health closely – seeking medical advice for symptoms of colon polyps and undergoing regular screenings, especially for those at risk, to catch and treat colon pathologies early.
Colon polyps primarily develop in individuals over 40, more commonly in men than women, and are uncommon in children.
Determining the exact prevalence and incidence is challenging due to many asymptomatic cases and the scarcity of preventive screenings, even among those at risk. Polyps are detected in 10-20% of the general population and two-thirds of individuals over 45 years old during post-mortem examinations.
Typically, these growths are located in the rectum and sigmoid colon, with occurrences in the colon being less common.
Colon polyps classification
According to the number of neoplasms in the colon, single and multiple polyps are distinguished.
According to the classification of polyps by morphological structure, colon polyps can be classified as:
- Adenomatous or glandular polyps are determined in 50% of patients with this pathology; they have the appearance of dense overgrowths of glandular epithelium of pinkish color, branching or mushroom-shaped, 2-3 cm in diameter; they do not usually ulcerate or bleed, but can be transformed into a malignant tumor.
- Adenopapillary polyps, sometimes malignant, are found in one in five patients.
- Papillary, or villous colon polyps, are found in 14% of patients with polyps. They have the appearance of nodules of red color, are rich in blood vessels, 4-5 or more cm in diameter, prone to bleeding and ulceration, and often transformed into cancer.
- Metaplastic or hyperplastic colon polyps are nodules of soft consistency, slightly elevated above the intestinal mucosa, up to 0.5 cm in diameter, and usually benign.
- Juvenile colon polyps are large and solitary, situated on a pedicle, and benign.
- Pseudopolyps arise from a chronic inflammatory process, benign.
Several types of polyps can be detected simultaneously in the same patient.
Symptoms of colon polyps
In many instances, colon polyps in both men and women are asymptomatic and discovered incidentally during examinations for other suspected conditions. When symptoms of colon polyps do occur, they may include:
- Abdominal pain that is aching, squeezing, or cramping in nature, with unclear location, often alleviating after bowel movements;
- Irregular bowel movements, such as constipation, diarrhea, or a combination of both;
- The appearance of mucus or blood in the stool;
- In cases of extended bleeding from the affected growth – symptoms like weakness, skin pallor, shortness of breath, rapid heart rate, anemia.
Causes of colon polyps
The exact causes of polyps in the colon are unknown. They are believed to be based on a chronic inflammatory process in the colon’s wall (enteritis, colitis, sigmoiditis, proctitis). Other provoking factors are:
- genetic predisposition
- age over 50
- irregular, unbalanced diet with a high content in the diet of red meat, easily digestible carbohydrates, fried, fatty, spicy, spicy, salty, smoked dishes, fast food, alcohol, deficiency in the diet of vegetable fiber – fresh fruits and vegetables
- smoking
- obesity
- sedentary lifestyle
- air polluted with industrial chemicals
Colon polyps diagnosis
Symptoms, patient history, and physical examinations for intestinal polyps often don’t provide specific clues that can lead directly to a diagnosis. The most effective diagnostic tools are fecal occult blood tests and endoscopic colon examinations, known as colonoscopy.
- A fecal occult blood test can detect even tiny amounts of blood in stool, suggesting unnoticed, symptom-free bleeding from the gastrointestinal tract. This may hint at mucosal damage, potentially from a bleeding intestinal polyp.
- A colonoscopy is the next step for pinpointing the bleeding source. In this combined therapeutic and diagnostic procedure, an endoscope equipped with a camera and light is inserted through the rectum into the intestine. As the device moves through the colon, the doctor examines the mucosal surface on a monitor, identifying the location, size, and number of any polyps, along with any signs of ulceration, bleeding, or potential cancerous changes. Tissue samples (biopsies) can be taken for further histological examination, and polyps may be removed during the procedure. To ensure patient comfort and reduce anxiety, the procedure can be performed under general anesthesia.
- Alternative diagnostic methods like sigmoidoscopy, virtual colonoscopy, and ultrasound are considered when colonoscopy is not an option, although they are generally less informative.
Colon polyps treatment
The only effective method of treatment for colon polyps is surgical intervention. The amount of surgery depends on the type, number, and size of the formations. The patient may be recommended:
- Endoscopic removal using a special loop with subsequent coagulation of the resulting mucosal defect
- Open removal of the polyp with preservation of the intestine
- Resection (removal) of a small section of the intestine in which the tumor is located
- Subtotal colectomy or partial removal of the colon is usually performed in hereditary familial polyposis.
All these treatment options are available in more than 704 clinics worldwide (https://doctor.global/results/procedures/colon-polypectomy). For example, colon polypectomy can be performed in five clinics across Singapore for an approximate price of $5.5 K (https://doctor.global/results/asia/singapore/all-cities/all-specializations/procedures/colon-polypectomy).
Removed polyps are necessarily sent for histologic examination to determine their morphologic structure and degree of malignancy. The outcome of this analysis influences the subsequent management strategy for the patient and their prospects for recovery.
Prevention of colon polyps
To reduce the risk of polyps in the colon, it is recommended to:
- follow a healthy diet (patient should minimize the use of fried, fatty, smoked dishes, red meat, and alcohol, and increase the content of fresh fruits and vegetables in the diet);
- stop smoking
- lead an active lifestyle, avoid hypodynamia
- timely diagnose and treat diseases of the digestive tract, especially the colon
- patients over 45 should undergo stool analysis for hidden blood and preventive colonoscopy at least once a year