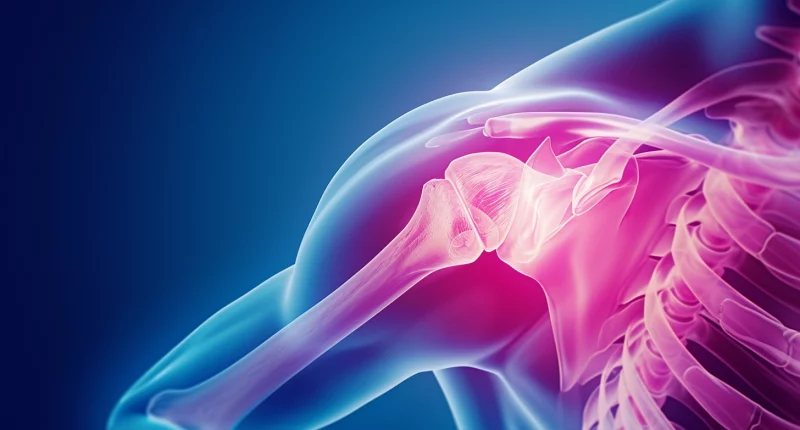
Clavicle Fracture
Overview
The clavicle, or collarbone, is a solid, slightly S-shaped bone that connects the breastplate (sternum) to the shoulder and is easily visible in many individuals. It forms a crucial part of the shoulder structure, attaching to the sternum at the sternoclavicular joint and connecting to the shoulder blade (scapula) at the acromion, forming the acromioclavicular joint. The clavicle acts as a strut, which is vital in linking the sternum to the shoulder blade, making it susceptible to fractures.
Clavicle fractures, which account for about 5% of all adult bone fractures, are commonly caused by significant force on the shoulder. This can happen through direct impacts, such as falling onto the shoulder or an outstretched arm. Such incidents place tremendous pressure on the bone, often causing it to snap or break. These fractures can be extremely painful and may severely limit arm movement.
Anatomy
The clavicle, also known as the collarbone, is a long, slender, S-shaped bone that lies horizontally across the front of the shoulder. It serves as a bridge between the sternum (breastbone) at the center of the chest and the scapula (shoulder blade) at the shoulder. This bone has two ends:
- The medial end connects to the sternum at the sternoclavicular joint.
- The lateral end connects to the scapula at the acromioclavicular joint.
Functionally, the clavicle:
- Acts as a support strut for the shoulder, allowing for a wide range of shoulder movements.
- Protects underlying nerves and blood vessels in the neck and shoulder.
- Serves as an attachment point for neck, back, and shoulder muscles.
Due to its location and functions, the clavicle is prone to fractures, especially from falls or impact injuries.
Classification of clavicle fractures
Medical experts commonly categorize clavicle fractures into three main types:
- Type I Fractures are midshaft fractures in the middle third of the clavicle, a region where the bone is flat and slender. Representing the majority of clavicle fractures, these are usually treated non-surgically.
- Type II Fractures: Also known as lateral or distal fractures, these occur at the end of the clavicle closest to the acromion, the shoulder’s bony projection. Comprising about 21 to 28% of clavicle fractures (although some estimates are lower), the approach to treating these fractures varies and may include surgery.
- Type III Fractures: These medial fractures are rarer, constituting roughly 2 to 4% of all clavicle fractures. They occur near the neck’s side of the clavicle. The treatment plan for these fractures is determined on a case-by-case basis and may involve surgical intervention.
Taking into account the condition of the skin in the area of trauma, two variants of fractures are distinguished:
- closed – the skin is intact;
- open – the skin is damaged (there is a wound).
Causes
The immediate cause of a clavicle fracture is associated with an injury whose force exceeds the strength of the bone tissue. Such fractures can occur in falls from heights, automobile accidents, and crushing the body between massive objects.
Symptoms
- pain of medium severity, which becomes incredibly intense when groping the injured area or when trying to lift the upper limb;
- swelling and bruising of soft tissues in the supraclavicular and subclavian region;
- forced position of the upper extremity – the patient supports the arm with the elbow joint;
Diagnosis
Physical Examination
During a physical examination for a suspected clavicle fracture, your doctor will inquire about the injury’s cause and your symptoms. They will closely inspect your shoulder, typically identifying a noticeable bump or deformity at the fracture site, where gentle pressure will cause pain. While it’s uncommon for bone fragments to pierce the skin, they may protrude, causing a tent-like appearance of the skin over the fracture. Additionally, your doctor will conduct tests to check for any nerve or blood vessel damage associated with the fracture.
Imaging
The main method of diagnosing a clavicle fracture, including a recurrent one, is a radiographic examination performed in 2 projections. Scanning is performed in a horizontal position of the patient, with the face turned to the side opposite the injured clavicle.
In intra-articular fractures, a CT scan is indicated. Layer-by-layer scans of the examined area allow you to detail the nature of the damage.
The examination program also includes electrocardiography, cardiac ultrasound, and Doppler ultrasound of the main vessels of the upper limb, which may be damaged in a clavicle fracture.
Treatment
Conservative methods are mostly used in clavicle fractures without displacement or with minor displacement of the fragments. The method of choice in treating displaced, fragmented, and unstable clavicle fractures is open repositioning and osteosynthesis with nails or plates of various modifications.
Non-surgical
- Arm Support: Immediately following the fracture, a simple sling is often used to provide comfort and keep the arm and shoulder properly aligned during the healing process.
- Physical Therapy: Despite some pain, maintaining movement in the arm is crucial to avoid stiffness in the shoulder and elbow. Patients typically start exercises to maintain elbow mobility right after the injury.
- Pain Management: Over-the-counter pain relievers like acetaminophen are commonly prescribed to alleviate discomfort during recovery.
Surgical
Surgery for clavicle fracture, in most cases, is categorized as high-tech and involves modern implants and advanced osteosynthesis techniques. Such interventions can ensure rapid patient recovery and return to the usual way of life, including during the fracture’s consolidation (fusion).
The most common surgical method is open reduction and internal fixation, involving repositioning the bone fragments to their original alignment and securing them with metal hardware. This typically includes:
- Plates and Screws: Bone fragments are aligned and fixed with screws and metal plates on the bone’s external surface. Post-surgery, a small area of skin numbness near the incision is normal but diminishes over time. The plates, often palpable under the skin, are usually not removed unless they cause discomfort.
- Pins or Screws: Used for maintaining the position of the fracture, these are generally removed after healing due to potential skin irritation.
Surgery aims to stabilize the fracture, reduce complications, and restore the clavicle’s functionality.
Clavicle osteosynthesis is performed in more than 793 hospitals worldwide (https://doctor.global/results/procedures/clavicle-osteosynthesis).
The estimated cost for private patients undergoing clavicle osteosynthesis is around 11,410 USD in South Korea ((https://doctor.global/clinic/korea-university-anam-hospital#prices). At the same time, in European countries such as the Czech Republic, the procedure is priced at approximately 6,000 USD (https://doctor.global/clinic/st-zdislava-hospital#prices).
Rehabilitation
Rehabilitation following a clavicle fracture typically involves several key components:
- Targeted Shoulder Exercises: These are specifically tailored exercises aimed at strengthening the shoulder girdle, prescribed by a rehabilitation specialist.
- Physiotherapy Treatments: These procedures enhance metabolism and microcirculation in the musculoskeletal system.
- Therapeutic Massage: This helps boost blood circulation in the fracture area and stimulates the muscles around it.