Pulpitis
Pulpitis is an inflammation in the inner connective tissue of the tooth (pulp), where the nerve and vascular bundle are located. Lack of treatment can lead to periodontitis, the gradual destruction of tooth tissue.
Symptoms
- Sharp tooth pain (increases at night).
- The pain radiates to the teeth nearby, ear, throat, and temple.It may be attack-like and may appear after eating hot or cold food.
- Presence of a dark carious cavity in the tooth.
Causes
As a rule, pulpitis is a complication of other diseases or a consequence of cracked, chipped enamel.
Caries
Carious bacteria penetrate the enamel, soften the dentin, and enter the pulp as a result of their activity. A dark cavity is most often visible on the upper part of the tooth.
Periodontitis
Infection can enter the pulp with blood and lymph flow through the opening in the lower part of the root (apical). Nerves and blood vessels pass through it. In this case, pulpitis and periodontitis may be combined.
Injuries
In rarer cases, typically at a young age, the infection enters the pulp through cracks in the dental hard tissue following trauma.
Classification
Pulpitis histological classification
Acute pulpitis
It is characterized by acute and excruciating pulp inflammation, which develops rapidly – within 1-3 days. The pain is mainly attack-like, temporarily relieved by painkillers.
Chronic pulpitis
The disease develops slowly over several months or even years. Long ” calm ” periods are replaced by periods of aching painful sensations lasting from 2-3 to 10-14 days. Periodically, exacerbations with acute pain and swollen gums are possible.
Gangrenous pulpitis
A neglected inflammatory process is accompanied by the dying off of the pulp tissue. Due to the lack of blood supply and nutrients, hard tissues gradually weaken and deteriorate. This process can be visually noticed by darkening inside the tooth. Inflammation is often accompanied by bad breath and an accumulation of exudate (fluid released during inflammation).
Fibrous pulpitis
This form is characterized by the growth of fibrous granulations in the inner dental cavity. Complaints include painful sensations during chewing and a feeling that the tooth spreads from the inside. As the granulation connective tissue grows, it cuts off the blood supply to the dental tissues and their access to nutrients. What follows is their gradual destruction. As a rule, fibrous pulpitis is chronic and develops over months.
Pulpitis Clinical Classification
Reversible Pulpitis
This condition implies that the tooth’s nerve can heal from a compromised state to a healthy one, provided it receives appropriate treatment.
Irreversible Pulpitis
In this case, the pulp has deteriorated to an extent where it’s beyond recovery and cannot heal itself. Consequently, the affected nerve must be extracted through a root canal procedure, as the tooth is either dying or may already be dead.”
Complications of pulpitis
We have repeatedly mentioned above that the development of this disease inevitably leads to the weakening and gradual destruction of dental tissues. The infection can affect deeper tissues, such as the jawbone, if untreated.
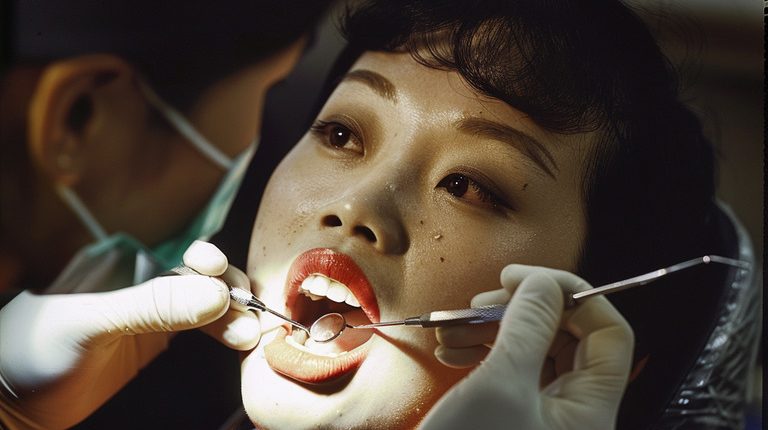
Diagnosis of pulpitis
The dentist examines the patient during the initial appointment. A targeted (in some cases, panoramic) x-ray is performed to assess the pulp’s condition. Based on the obtained image, the doctor concludes the possibility or impossibility of treating the affected tooth.
Pulpitis treatment
Preparation
In preparation for manipulation, it is obligatory to clean tartar with ultrasound. The deposits are a source of infection and often conceal carious lesions.
Anesthesia
Doctors carry out all therapeutic manipulations exclusively after the introduction of infiltration anesthesia. The drug and dose are selected individually. So that the patient does not feel the injection, the dentist pre-treats the gum with an application anesthetic. Afterwards, the procedure is entirely painless.
Pre-endodontic procedures
In most cases, treatment begins with the treatment of carious lesions. The doctor uses magnifying optics to remove infected tissue and works directly with the pulp.
Treatment of dental pulp
Treatment of pulpitis with complete pulp preservation
If the patient comes to the clinic in time, and pulpitis is at the initial stage of development, there is a chance to save the pulp. The doctor opens the tooth cavity, puts a treatment material on the pulp or into the pulp, and applies a temporary filling.
The doctor removed the temporary filling during the second visit and evaluated the result. If it is positive, the tooth is restored with light-curing polymer materials.
Treatment of pulpitis with partial pulp preservation – pulpotomy
The method is used for multi-rooted teeth in cases where the infection mainly affects the upper part of the pulp-pulp chamber. The doctor gains access to the dental cavity and root canals, and only inflamed tissue from the pulp chamber and root canal orifice is removed. After thorough antiseptic treatment, a therapeutic preparation is put into the tooth cavity, and a temporary filling is placed.
In the second stage, the dentist evaluates the successful treatment manipulations and restores the dental tissue by placing a permanent filling.
Pulpitis treatment with complete pulp removal – pulpectomy
Procedures are carried out in cases where the infection has significantly spread into the root canals, and there is no chance to save the affected pulp.
- Vital extirpation is performed in one visit to the clinic and is indicated for acute pain management and emergency relief of inflammation. The tooth is isolated from saliva with an elastic plate – cofferdam. The doctor treats the carious cavity, opens and expands the tooth cavity, and removes the pulp completely from a chamber and canals.
- Devital extirpation is performed in two visits and is mainly indicated for the treatment of chronic forms of pulpitis. After removing carious lesions and opening the tooth cavity, the doctor treats its upper part with an antiseptic solution and deposits necrotizing paste (arsenic or paraformaldehyde) into the pulp. An anesthetic drug is also put in. After that, the tooth cavity is filled, and the patient goes home. After 1-2 days, the tooth cavity is opened again, and the pulp is removed.
After removing the pulp, the dentist works with the root canals, eliminating pathological tissues and conducting antiseptic treatment. Then, the canals are sealed with gutta-percha pins. The tightness is checked on an X-ray. After that, the restoration of dental tissues with filling material is started.
Pulpitis can be treated by any of the methods mentioned above in 261 clinics worldwide (https://doctor.global/results/diseases/pulpitis). Treatment per one dental canal starts from 19 $(https://doctor.global/results/procedures/root-canal-treatment-per-canal).
Contraindications to treatment
Therapeutic manipulation should be postponed if the patient has:
- have infectious diseases
- exacerbated a chronic illness
- recent (less than six months ago) heart attack and stroke
However, these contraindications do not apply to complex cases where the infection seriously threatens the patient’s health, and treatment is urgent.
If the disease is too advanced, it is pointless to treat the tooth, and it will have to be extracted due to a large degree of root destruction.
Prevention of pulpitis
The development of pulpitis can be avoided by following some simple recommendations:
- not to neglect oral hygiene
- avoid traumatic factors (chewing nuts, breadcrumbs)
- visit the dentist every six months for hygiene and preventive chek-up