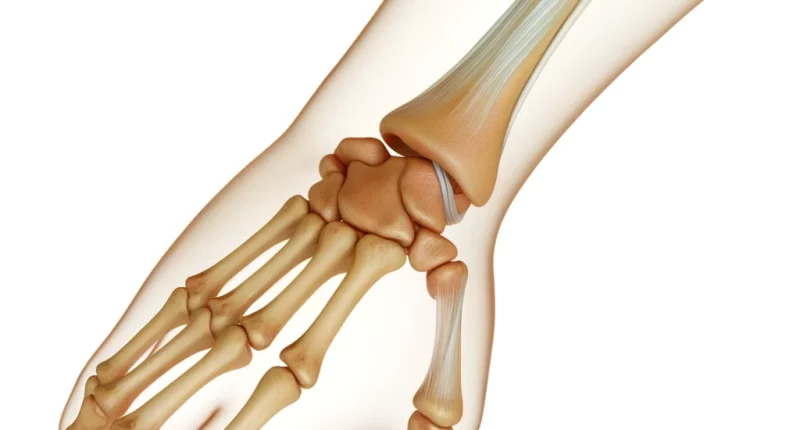
Ganglion cyst of the wrist and hand
What does that mean?
A ganglion cyst of the wrist and hand, or as it is also called, a hygroma, is a cystic benign mass emanating from the joint capsule or tendon sheath.
About the disease
A synovial cyst is a unicompartmental or multicompartmental fluid mass with minimal connection to the underlying lymphatic system. In Greek, “hygroma” means “tumor containing fluid.”
Cystic formations result from trauma, resulting in local hypoxia of the injured tendon or synovial bag with disruption of intercellular connections in this area. It leads to the start of a cascade mechanism – free-radical oxidation, acting destructively on connective tissue.
Hygroma (tendon ganglion), according to the International Classifier of Soft Tissue Pathologies, is a benign mass developing from the joint capsule or tendon sheath. The wall of this cyst is formed by dense connective-tissue fibers (the inner layer is lined with fibroblasts). The formation can be single- or multi-chambered. Inside the hygroma is a jelly-like substance of a yellowish color.
As practice shows, more than 60% of people who went to the doctor about tumor-like formations were diagnosed with hygroma. The size of hygromas varies considerably and can reach 10 cm, but their growth usually stops at 2-4 cm. Most often, the pathological process is found in the area of the wrist joint; somewhat less often, they are localized in the area of the fingers of the hand or elbow and in the area of the foot or knee on the leg.
Treatment is determined by the localization and size of the hygroma. Two tactics are used – conservative (puncture of the mass) and operative (radical removal by classical, laser coagulation, and other minimally invasive methods).
Types of hygromas
The following types of hygromas are distinguished:
- isolated – has no connection to the parent joint sheath;
- valve – fluid from the hygroma cannot flow back into the joint bag;
- communicating – the junction between the hygroma and the articular bag is functioning;
In the latter case, fluid from the hygroma cavity periodically escapes into the articular bag but may subsequently return to the lumen of the hygroma (the “hourglass” phenomenon in articular hernia). It creates a false impression of self-healing.
Symptoms of hygroma
The main symptoms of hygroma:
- cosmetic discomfort consisting of the presence of a tumor-like mass;
- discomfort in performing everyday activities at home or at work;
- mild to moderate pain (however, one in three patients has no pain).
In most cases, pain occurs when the hygroma is pressed or bruised. It is believed that hygroma rarely compresses vessels and nerves, so the patient is not bothered by significant pain.
What does the pathologic focus look like? The skin over the mass is not changed in all cases; color and skin temperature do not differ from normal. The mobility of the hygroma is weakly expressed, with palpation showing a tight elastic consistency (medium between hard and soft consistency). Attention is drawn to the close localization of the hygroma to one of the joints. The function of the mobile joint, near which the hygroma is located, is most often not disturbed, but as the cystic formation grows, patients notice discomfort during movements or even pain when trying to maximize flexion/extension in the joint.
Localization of hygroma on the palm surface of the hand (wrist) near the direction of the median or ulnar nerve can lead to compression of these nerve trunks, accompanied by moderate pain and numbness of the fingers in the zone of their innervation.
Causes of hygroma
Hygroma formation is most often associated with prolapse of the synovial membrane from the joint cavity, which can be caused by traumatic or inflammatory factors: damage to the joint capsule, arthritis, and bursitis. Thus, the main causes of hygroma are traumatic impact or inflammatory lesions. Under the influence of the damaging factor, the tissues of the tendon or synovial bag receive insufficient oxygen. Local hypoxia leads to the formation of free radicals. The latter destroys connective tissue, which is poor in antioxidant enzymes. Hypoxia stimulates explicitly the function of fibroblasts, which begin to divide actively. As a result, fibroblasts produce large amounts of glycosaminoglycans, which are the main component of the fluid that fills the hygroma cavity.
Risk factors include:
- superficial localization of the tendon sheath or synovial bursa;
- repetitive work involving increased stress on joints or tendons.
There is an assumption of genetic predisposition to the development of hygromas. Thus, in families where parents suffer from this pathology, children also often face this problem. Sometimes, hygroma can form during pregnancy due to structural changes in connective tissue induced by gestational hormones.
Diagnosis of hygroma
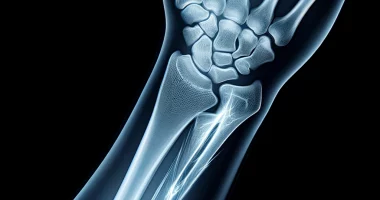
According to clinical recommendations, the diagnosis of hygroma is based on the assessment of complaints, objective examination data, and the results of the use of instrumental methods of investigation.
- Ultrasound scanning – allows you to determine the size of the mass, its location, and its relationship to large vessels, which is especially important when planning surgical intervention. The advantage of ultrasound is the ability to identify the hygroma’s pedicle and visualize the site of origin of the cyst.
- X-rays can be used to determine the contours of the hygroma and its relationship to surrounding bone structures.
- Magnetic resonance imaging (MRI) or computed tomography (CT) – allows the identification of more detailed features important for differential diagnosis. MRI is likely indicated when evidence from ultrasound and radiologic examination is inconclusive. MRI provides an opportunity to visualize the communication of the hygroma with the joint cavity
Hygroma treatment
Modern medicine considers two methods of treating hygromas: conservative, which involves various puncture options, and surgical removal of the hygroma, which is considered a radical way to remove it.
Conservative treatment
Conservative therapy utilizes various methods of puncture interventions for hygromas:
- puncture the mass and aspirate the contents;
- puncture with subsequent injection into the cavity of the hygroma hormonal agents, cytostatics;
- laser obliteration of synovial hygroma;
Between puncture, tight elastic bandaging and longitudinal joint immobilization may be recommended.
Surgical treatment of hygroma
Failure of conservative treatment is considered an indication of surgical intervention as a radical method of treatment. The basis of surgery for hygroma is the removal of the cyst with suturing of its pedicle to eliminate communication with the lumen of the joint or tendon sheath. In cases where the hygroma loses communication with the joint cavity, simple removal of the hygroma is indicated.
The hygroma communicates with the joint cavity via the pedicle. Therefore, this communication must be eliminated during surgery (this reduces the risk of recurrence of the hygroma). In some cases, cystic formations are close to the artery. Therefore, when performing surgical intervention, surgeons perform all manipulations with utmost precision and care, especially when isolating the hygroma stem, when there is a risk of damage to the artery with the possibility of bleeding.
All these treatment options are available in more than 800 hospitals worldwide (https://doctor.global/results/diseases/ganglion-cyst-of-the-wrist-and-hand). For example, Hand ganglion cyst removal can be performed in 40 clinics across Germany for an approximate price of $4.4 K(https://doctor.global/results/europe/germany/all-cities/all-specializations/procedures/hand-ganglion-cyst-removal).
Hygroma prevention
The main direction of hygroma prevention is the prevention of traumatism and inflammatory lesions of the joints. In case of injury or arthritis, it is vital to seek qualified medical assistance from a traumatologist promptly.
Rehabilitation after a hygroma
After hygroma in the postoperative period, rehabilitation involves the creation of rest for the operated limb, using a bandage for immobilization, and releasing the patient from physical exertion for 4-6 weeks.