Hip Osteoarthritis
What’s that?
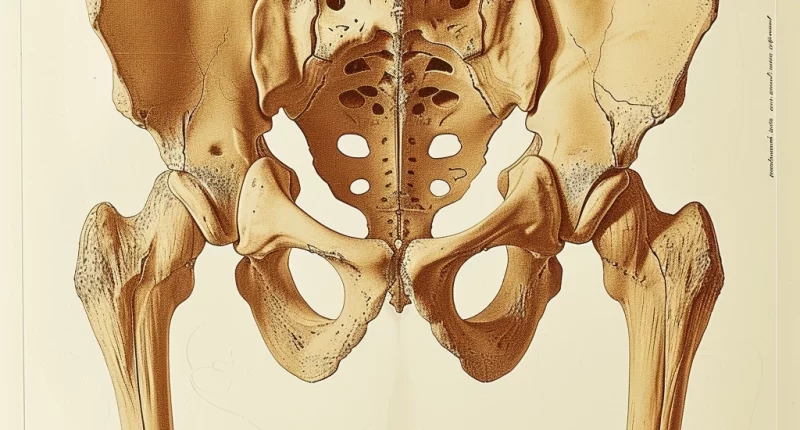
Osteoarthritis of the hip (or coxarthrosis) is a destructive change in the articular cartilage, exposing the underlying bone. The disease is characterized by bony overgrowths (osteophytes) that develop due to associated degeneration.
About the disease
The pathological process affects all joint structures, including ligaments and muscles, increasing inflammatory reactions. Coxarthrosis symptoms usually include joint pain, stiffness, and decreased range of motion. However, clinical manifestations may not always be present, even though radiologic changes may be. In addition, symptoms are characterized by a certain cyclicity. The disease is equally common in men and women, and in 1/3 of cases, it is bilateral (right and left-sided).
Predisposing risk factors for osteoarthritis are well known and include older age group, increased body fat, traumatic joint injury, bone structure, and family history. The prevalence of the disease is steadily growing as the world population is progressively aging. Previously, at 70 years and older, the disease occurs in an average of 90% of cases. However, recently, there has been a trend towards rejuvenation of osteoarthritis globally. According to the latest data on the prevalence of the disease, by the age of 50 years, the pathology is observed in one in three inhabitants after 70 years – in all. The disease is initially asymptomatic and often slowly progresses.
Diagnosis of coxarthrosis is based on imaging studies – radiography, ultrasound scanning, or magnetic resonance imaging. Treatment depends on the stage of the pathological process and can be conservative or surgical.
Types of hip osteoarthritis
From the etiologic point of view, the following types of hip osteoarthritis are distinguished:
- Primary – has an unclear origin. In most cases, this pathological process begins unilaterally. Further, the process spreads to the opposite joint.
- Secondary – which results from trauma (post-traumatic), dysplasia of the hip joint (dysplastic), endocrine, metabolic disorders, and infectious and non-infectious arthritis.
Considering the prevalence of pathological changes, primary osteoarthritis is divided into localized and generalized.
Symptoms of coxarthrosis
The primary clinical manifestation of hip osteoarthritis is pain in the groin area. Usually, the pain syndrome irradiates in an upward direction. Pain sensations can be localized along the anterolateral part of the thigh and in the knee area. In some cases, the gluteal region can hurt. The peculiarities of irradiation determine the diagnostic difficulties.
Another manifestation is considered to be stiffness of movement in the hip joint, which occurs after a period of rest. Over time, the mobility of the lower limb is also limited. The first to suffer are external abductions, lifting the leg upward. It becomes challenging to put on shoes and socks; the patient practically cannot sit facing the back of a chair (it is difficult to spread the legs wide). During movement, a slight crunch can be detected. Osteoarthritis can be accompanied by inflammation of the articular capsule near the acetabulum. In this case, there is pain on the lateral surface of the joint.
In later stages, lower limb shortening develops because the femoral head is not in the correct position. The change in the length of the affected leg predisposes to claudication. If there is a bilateral lesion, the so-called duck’s gait appears. With the prolonged existence of the disease, secondary atrophy of the thigh and gluteal muscles occurs. Clinically, this is manifested by such a symptom as lowering the pelvis when leaning on the affected leg.
Causes of hip osteoarthritis
Recently, the causes of coxarthrosis have been attributed to genetic predisposition. Thus, in 60% of cases, hip osteoarthritis is inherited. Some cases of familial osteoarthritis may be associated with mutations encoding the synthesis of collagen molecules. However, the influence of other risk factors such as gender, obesity, and previous traumatic injury to the joint also play a role in the development of the disease.
To date, many authors believe that osteoarthritis is caused by various factors: mechanical, neurotrophic, vascular, endocrine, and age-related, as well as having a genetic and constitutional predisposition, but the actual causes have yet to be definitively established. The pathological condition of the synovial capsule and fluid also plays a significant role in osteoarthritis, due to which degenerative changes in cartilage occur, and cold and high humidity are considered predisposing factors. In some cases, the development of the disease may be associated with high-impact sports (cases of osteoarthritis in soccer players, handball players, hockey players, weightlifters, and track and field athletes running long distances).
The disease may have a different prognosis, which is determined by the pathologic process’ progression rate. Progressive destruction of the femoral head and aggravation of the process of degenerative-dystrophic changes are associated with an increase in the size of the femoral condyle with increasing dystonia of the lumbosacral muscle. Patients with these features are at risk and are potential candidates for early prosthetic replacement.
It is believed that in primary osteoarthritis, there is a pronounced thinning of bone tissue. The predominance of fibrotic changes in hyaline cartilage characterizes secondary forms of the disease.
Diagnosis of coxarthrosis
Additional imaging is required to establish a definitive diagnosis, which allows a clear assessment of pathological changes in the joint.
- Radiography.
X-ray criteria for coxarthrosis include a decrease in the height of the joint gap, bone thickening in the subcartilaginous zone, and bone overgrowths. Radiographic scanning of the left and right joints is carried out, allowing you to compare the condition. Based on the obtained data, the Kellgren-Lawrence stage of the pathologic process is determined.
- Magnetic resonance imaging.
MRI is considered a method of early detection of hip arthrosis. MRI examinations allow assessment of the condition of all joint structures – cartilage plate, subcartilaginous bone zone, soft tissue, and synovium.
- Ultrasound scan of the joint.
The method allows you to detect the initial signs of degeneration of joint structures and assess the state of the ligamentous and tendon-muscular compartments. At the same time, ultrasound has limited opportunities for studying bone tissue (radiography will help to answer this question).
Hip osteoarthritis treatment
Treatment of coxarthrosis is a challenging task. In some cases, a comprehensive conservative approach is sufficient; surgical intervention is required in other cases.
Conservative treatment
Conservative management tactics are usually recommended in the initial stages of the disease. This approach consists of 2 components:
- non-medicamentous, represented by orthopedic constructions that unload the joint, the performance of therapeutic and recreational exercises, reduction of excessive weight, physical procedures, and similar measures;
- medication, which is primarily aimed at controlling the pain syndrome (this is achieved with anti-inflammatory nonsteroid drugs, myorelaxants, and neuroblockers).
If deforming arthrosis is complicated by bursitis or synovitis, then local application of injectable corticosteroids is possible.
Given the quantity and quality of synovial fluid changes in osteoarthritis, intra-articular injection of various forms of natural and synthetic synovia prostheses has recently been widely used. As a result of such manipulation, the amplitude of movement increases, and the pain syndrome is controlled. This is due to a decrease in the friction force of hyaline cartilage and an improvement in the shock-absorbing function of the joint.
However, if, despite the applied therapeutic measures, the joint develops deformity, the question of surgery for coxarthrosis (hip arthroplasty) is decided.
Surgical treatment
Today, there are many different types of endoprostheses. A distinction is made between cemented, cementless, and hybrid endoprostheses. In practice, the cementless endoprosthesis is used much more, approximately 80%; the remaining 20% are cemented and hybrid prosthetics. An orthopedic traumatologist can help you choose the optimal option.
All these surgical treatment options are available in more than 950 hospitals worldwide (https://doctor.global/results/diseases/hip-osteoarthritis). For example, Total hip replacement can be performed in 24 clinics across Turkey for an approximate price of $12.6 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/total-hip-replacement-unilateral).
Prevention of coxarthrosis
Prevention of coxarthrosis consists of the following:
- controlling body weight and keeping weight within normal limits;
- performing physical exercises according to the correct technique;
- preventing injury to the hip joint as much as possible;
- prophylactic taping.
However, only sometimes, even the strictest compliance with these recommendations can prevent the development of the disease, especially if the patient is in the risk group due to aggravated heredity. In such a situation, early diagnosis of coxarthrosis and a comprehensive therapeutic program that will reduce the risks of deforming changes are essential.
Rehabilitation for hip osteoarthritis
Rehabilitation for hip osteoarthritis includes the following areas:
- physical therapy;
- electrical muscle stimulation;
- taping;
- massage.