Interstitial lung disease (ILD)
Definition
Interstitial lung disease is a group of diseases that occur with the development of diffuse inflammation of the lung stroma, mainly bronchioles and alveoli. Symptoms of such changes are fever, general malaise, weight loss, non-productive cough, dry inspiratory wheezes, pulmonary insufficiency (dyspnea, tachypnea), and right ventricular heart failure. The diagnosis of interstitial diseases is confirmed by the data of radiography and CT lungs, the study of external respiratory function, and lung biopsy. Steroid therapy (or cytostatic), bronchodilators, and oxygen therapy are prescribed as treatment.
General information
Interstitial lung diseases (ILD) are various lung lesions, the pathomorphologic basis of which is chronic diffuse inflammatory infiltration of alveoli, small bronchi, and pulmonary capillaries with the outcome of fibrosis. ILD includes 130 diseases of clear and unclear etiology. In patients hospitalized in pulmonology departments, one or another interstitial lung disease is diagnosed in 10-15% of cases. The predominant contingent of patients are men aged 40-70 years, in most cases smokers. Some diseases of this group have reversible course and relatively favorable prognosis; others lead to early disability and even death.
Classification of interstitial lung diseases
The classification of ILD, developed in 2002 by the American Thoracic Society (ATS) and the European Respiratory Society (ERS), is accepted as a basis. According to this classification, interstitial lung diseases are distinguished:
1. With an established etiology:
- Drug, radiation, toxic ILDs
- HIV-associated pneumomycoses
- ILD against the background of collagenosis (scleroderma, dermatomyositis, rheumatoid arthritis, SLE) and pneumoconioses (asbestosis, silicosis, berylliosis)
- ILD against the background of infections (SARS, disseminated pulmonary tuberculosis, pneumocystis pneumonia, etc.).
- ILD on the background of exogenous allergic alveolitis
2. Idiopathic interstitial pneumonias:
- Nonspecific, desquamative, acute, lymphoid, cryptogenic organizing;
- idiopathic pulmonary fibrosis
3. Granulomatous:
- ILD against the background of sarcoidosis, Wegener’s granulomatosis, pulmonary hemosiderosis, exogenous allergic alveolitis
4. Associated with other diseases:
- liver pathology (chronic hepatitis, primary biliary cirrhosis), intestinal pathology (nonspecific ulcerative colitis, Crohn’s disease), chronic renal failure
- hereditary diseases (neurofibromatosis)
- malignant tumors
5. Others:
- associated with histiocytosis X, lymphangioleiomyomatosis, pulmonary proteinosis, and primary pulmonary amyloidosis.
Pathomorphologic classification of interstitial lung diseases distinguishes the following types of interstitial fibrosis: simple, desquamative, lymphocytic, giant cell, and bronchiolitis obliterans with pneumonia.
Causes of interstitial lung disease
To date, the etiologic mechanisms of most ILDs remain unclear. We can reliably speak only about the causes of interstitial lung diseases with a known etiology. These include inhalation of inorganic substances, organic dust, mercury vapor, intake of toxic drugs, and radiation therapy.
Recurrent bacterial, fungal, and viral pneumonia, respiratory tuberculosis, respiratory distress syndrome, and bronchoalveolar cancer may be the basis for developing ILD. In addition, interstitial lung diseases can accompany collagenosis, blood diseases (hemolytic anemia, thrombocytopenic purpura, chronic lympholeukosis), hereditary diseases, etc. The most significant risk factor for CHD is smoking.
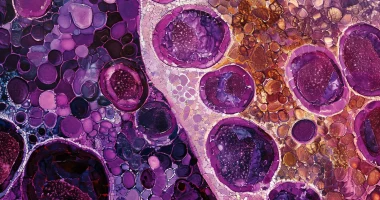
The pathogenesis of interstitial lung disease distinguishes acute, chronic, and terminal stages. In the acute stage, the lesion affects pulmonary capillaries and alveolar epithelium, and intra-alveolar edema develops. During this period, changes or progression may be completely reversible. In the transition of ILD into a chronic course, extensive lung damage (widespread fibrosis) is noted. In the terminal stage, fibrous tissue replaces the alveoli and capillary network completely, resulting in the formation of enlarged cavities (lung in the form of “bee honeycomb”).
Symptoms of interstitial lung disease
Despite the diversity of etiologic forms of ILD, their clinical course is largely similar and characterized by common and respiratory symptoms. The disease often begins subtly, and manifestations are vague and nonspecific.
General symptoms may include fever, malaise, rapid fatigue, and weight loss. A determining role in the clinical picture of interstitial lung disease are signs of respiratory failure. The earliest and most constant symptom is dyspnea: at first, it occurs or increases only on exertion, then becomes constant and progressive. Dyspnea is usually inspiratory and accompanied by wheezing, which may be mistaken for bronchial asthma.
A characteristic symptom of ILD is a nonproductive cough, dry or with scanty mucous sputum. Chest deformities occur frequently. In severe forms, pulmonary and cardiac failure develops.
Diagnosis of interstitial lung disease
When examining the patient, the pulmonologist notes tachypnea and inconsistency of dyspnea severity with physical changes in the lungs. During auscultation, crepitating rales of different localization are heard on inhalation. In the blood, moderate leukocytosis and increased ESR are noted; according to ELISA, serologic tests for antibodies to mycoplasma, legionellae, and rickettsia are negative. Blood gas and acid-base composition are analyzed (arterial hypoxemia in the early stages is replaced by hypercapnia in the terminal stage).
X-ray methods (radiography and CT of lungs) are of great informational value in diagnosing interstitial lung diseases. At early stages on X-rays and tomograms, it is possible to see deformation and strengthening of the pulmonary pattern, small focal shadows, and decreased transparency of lung fields (the phenomenon of “ground-glass opacity”); in the future, the radiologic picture of interstitial fibrosis and the picture of “honeycomb lung” develops.
According to spirometry data, restrictive types of pulmonary ventilation disorders and decreased lung volumes are more often detected. In the development of pulmonary hypertension, ECG reveals myocardial hypertrophy of the right heart compartments. Diagnostic bronchoscopy allows bronchoalveolar lavage; in ILD, neutrophils predominate in bronchial lavage waters. In addition, during endoscopic examination, a transbronchial lung biopsy can be performed. Open ortransthoracic biopsy of lung tissue is also performed in some cases.
Treatment and prognosis of interstitial lung disease
The first step in the treatment of ILD should be the refusal to smoke and interact with harmful industrial factors and toxic drugs. All subsequent therapy is carried out in parallel with treating the underlying disease.
In most cases, the first-line drugs in interstitial lung diseases are corticosteroids, prescribed in high doses for 1-3 months, followed by switching to maintenance doses. In the absence of positive dynamics within a year, cytostatics are prescribed. Bronchodilators (intravenous and inhaled) are used among other pharmaceuticals but are effective only at reversible bronchial obstruction. Oxygen therapy is indicated in arterial hypoxemia (RaO2 <50-55 mm Hg). In the case of severe interstitial lung disease, the only effective method may be lung transplantation.
The outcomes of ILD can be improvement, stabilization of the condition, progression of pulmonary fibrosis, fatal outcome, or — less often—spontaneous regression of changes (for example, in nonspecific interstitial pneumonia). Prevention of interstitial lung diseases is possible only in cases of known etiology.
You can find all the hospitals, that perform lung transplantation here:
https://doctor.global/results/diseases/interstitial-lung-disease-ild