Joint dislocation
A dislocation is a disturbance in the relationship between the articular ends of bones when they move beyond the anatomical limits of articulation.
About the disease
The main cause of bone dislocation is traumatic impact, which leads to damage to the ligamentous apparatus of the joint. The risk of dislocation increases against the background of dysplastic changes in connective tissue. In children, such injuries can also be congenital, which are associated with the peculiarities of the intrauterine period and childbirth.
Dislocation is manifested by intense pain, which increases when trying to move. Pain sensations are localized in the injured area. Dislocation is also characterized by impaired mobility of the joint – active movements that obey the patient’s will become impossible, while passive movements (performed under external influence) are accompanied by a springy effect.
The final diagnosis of this pathology is based on the data of radiographic examination. What does a dislocation look like on an X-ray? An important diagnostic sign is the displacement of the bone outside the joint cavity (the articular end of the bone is determined in an atypical place). In complex clinical cases, a layer-by-layer study of the pathologically altered area is performed using computerized or magnetic resonance imaging.
Depending on its localization, severity, and concomitant pathology, dislocation can be treated conservatively or operatively. Conservative tactics include adequate anesthesia (if necessary, additional muscle relaxation), manual repositioning of the displaced bone, control radiographs to assess the adequacy of repositioning, and subsequent fixation of the restored joint in a physiologic position with a plaster cast or bandage. In some cases, surgical intervention is indicated.
Types of dislocation
According to the classification, there are two types of dislocation:
- Acute – occurs at the time of injury that is indicated;
- Chronic is a recurrent dislocation in which instability develops in the joint.
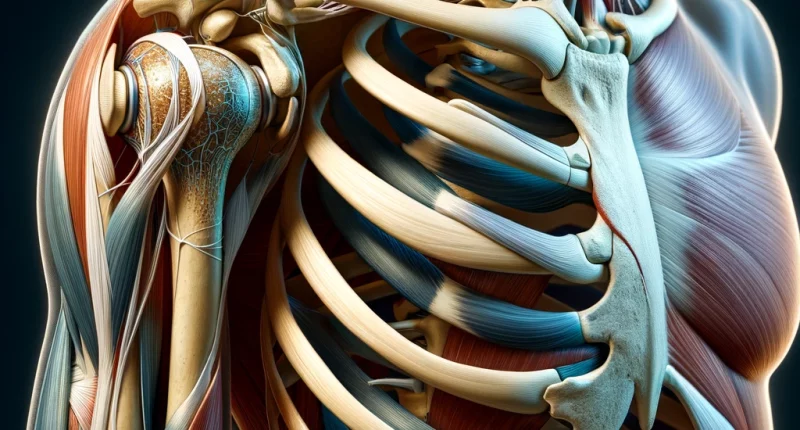
In terms of localization, the types of dislocations can be as follows:
- Dislocations of the arm and girdle of the upper limb – clavicle, in the area of the shoulder joint, elbow joint, and hand, fingers;
- Dislocations of the leg – in the hip joint, knee joint, patella (kneecap), ankle (involving the ankles), foot;
- Dislocations in the skull region when the lower jaw is affected (dislocation occurs in the temporomandibular joint);
- vertebral dislocations.
Clinical signs of joint dislocation
Clinical signs of dislocation may include the following:
- pronounced painful sensations in the injured area;
- soft tissue swelling;
- bleeding in the skin and subcutaneous tissue (bruising);
- visually detectable abnormality in the shape of the joint;
- inability to make voluntary movements in the joint;
- restriction of passive movements and a sensation of springy recoil;
- snapping sensation at the time of injury;
- pallor and coldness of the skin below the injured joint (a non-permanent sign, its appearance is associated with the impingement of feeding arteries);
- numbness of the skin and paresthesias (these symptoms are also not permanent; they are associated with compression of a major nerve trunk).
Reasons
Sprains can have the following nature of origin:
- traumatic – bone displacement occurs under the influence of an external force (direct or indirect);
- congenital – caused by intrauterine pathology of the joints, resulting in a decrease in their strength reserve;
- secondary – develops against the background of acquired musculoskeletal system pathologies (chondroplasia, tumor processes, tuberculosis infection, etc.).
Injuries are the most common cause of sprains. They can occur in everyday life, at work, in sports, and automobile driving. Traumatic impact can be realized during a direct blow to a limb or other body part, during a sharp contraction of muscle masses, during unnatural flexion and extension of a mobile joint, or violent pulling of an arm or leg.
Diagnosis of dislocations
Objectively determined signs of dislocation in the joint (joint deformation, swelling, lividity) in combination with complaints and anamnestic data (first of all, the fact of traumatic impact) allow the establishment of a preliminary diagnosis. However, its confirmation requires visualization of the pathologically altered area. It allows not only to assess the nature of the joint damage, but also to exclude a concomitant fracture. In most cases, the final diagnosis of dislocation is based on the data of radiographic examination. However, in about 5% of cases, this method does not allow the correct diagnosis to be established. How to recognize a dislocation in these difficult cases? Layer-by-layer scanning with CT or MRI comes to the rescue.
Treatment of dislocation
In most cases, dislocation is treated with conservative methods. If manual repositioning is not possible, surgical intervention is indicated.
Conservative treatment
Conservative treatment of dislocation involves adequate anesthesia, which eliminates pain and relaxes the muscles, creating conditions for repositioning the dislocated bone. However, additional medication relaxation is required in those areas with a pronounced muscle mass.
The next step is to recreate the anatomy of the joint. For this purpose, manual techniques are used to return the bone to its anatomically correct place. The result of such actions is evaluated with the help of X-rays. Once it has been confirmed that the manual repositioning has been successful, a plaster cast or bandage is applied.
Surgical treatment
Surgery for this pathology is recommended in the following cases:
- along-standing dislocation, when the bones “get used” to being in the wrong position;
- a combination of dislocation and fracture;
- certain dislocation localizations where surgical intervention is preferable (e.g., shoulder dislocation, given the long – up to six months – recovery period after manual repositioning);
- non-adjustable dislocations, when the muscular-ligamentous compartment between the displaced bones is pinched.
Surgery for dislocations can be performed either open or arthroscopic. The latter option is considered less invasive and is characterized by a short rehabilitation period. However, not all types of dislocations can be treated arthroscopically.
All these treatment options are available in more than 830 hospitals worldwide (https://doctor.global/results/diseases/joint-dislocation). For example, joint dislocation reduction can be done in 29 clinics across Turkey for an approximate price of $3.5 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/joint-dislocation-reduction).
Prevention
Dislocation prevention is aimed at preventing household, sports, and industrial injuries. For this purpose, it is recommended to ergonomically perform physical exercises and use protective equipment when engaging in traumaticactivities. Observance of traffic rules and the use of seat belts is also of great importance. Be extremely careful when traveling in icy conditions, and do not go outdoors unnecessarily.
Rehabilitation
After the plaster cast is removed, the active rehabilitation phase begins. Rehabilitation usually consists of the following areas:
- development of the joint with physical therapy methods;
- undergoing a course of rehabilitative massage;
- physiotherapy treatment;
- taping;
- electrical muscle stimulation.