Testicular cancer
What is testicular cancer?
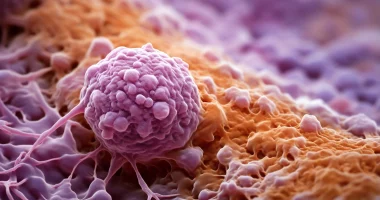
Testicular cancer is a cancerous disease in which a malignant neoplasm is formed from the epithelial tissues of the male sex glands.
Testicular cancer accounts for up to 2% of all malignant tumors and up to 5% in the structure of oncourological diseases. There are three age peaks of diagnosis – in boys under ten years of age, in men of reproductive age 25-40 years, and in the older age group (after 65 years). In most cases, only one testicle is affected. Bilateral cancer accounts for no more than 3% of cases.
Testicular cancer is considered a sufficiently aggressive oncologic pathology, prone to rapid development and early appearance of metastases. Early diagnosis of the disease and timely and comprehensive treatment with the help of modern methods contribute to the achievement of stable remission.
Stages
Based on the features of development, four stages of testicular cancer are distinguished:
- The first – pathological changes affect only the testicle. The tumor is not visible visually but is detected by palpation.
- The second – the diameter of the tumor is 2-5 cm. The tumor is detected not only palpatory but also visually, as it changes the shape of the scrotum. Regional lymph nodes may be involved.
- Third – the malignant process affects the testicular appendages, and the risk of metastases in distant lymph nodes increases.
- Fourth – the tumor infiltrates nearby tissues, and there are metastases in distant organs.
The disease is staged according to the international classification (TNM) according to the following criteria:
- T – features of tumor growth;
- N – presence of metastases in lymph nodes;
- M – metastases to distant organs.
Symptoms
In the initial stages of development, testicular cancer does not manifest itself in any way. As the mass grows, the patient can detect it palpatory. As a rule, malignant tumors are felt as a painless induration in the structure of one of the genital glands.
Due to the progression of the pathological process, the density of the testicles may change. An enlarging tumor provokes asymmetry of the scrotum. Large formations squeeze the nerve endings, which leads to the appearance of dull, aching pain in the scrotum and suprapubic area. A painful infiltrate or fluid accumulation in the scrotum may occur.
In advanced stages, testicular cancer is manifested by pain that occurs during urination and defecation, discomfort in the groin, enlargement of lymph nodes, as well as symptoms from other organs (which depend on the localization of metastases). Systemic manifestations of cancer pathology include weakness, fatigue, and exhaustion of the body.
Reasons
The exact causes of testicular cancer have not been established. The pathology is considered multifactorial. The disease is associated with cryptorchidism, congenital benign testicular neoplasms, and cases of testicular cancer in male blood relatives.
The following conditions have been recognized as risk factors:
- scrotal trauma;
- bad habits;
- exposure to ionizing radiation;
- hypodynamic lifestyle;
- regular overheating of the testicles, including heated car seats;
- trophic disorder of the scrotal organs;
- contact with carcinogens due to occupational activities, etc.
Diagnosis
A urologist may suspect testicular cancer during a physical examination. The tumor is usually detected by palpation of the scrotum and diaphanoscopy (scrotal imaging). Differential diagnosis is made using the following methods:
- General clinical tests (general blood and urine tests);
- tests for serum cancer markers;
- Ultrasound of the scrotal organs;
- MRI of the scrotum and pelvis.
The degree of tumor spread and involvement of regional lymph nodes are determined during the examination. Ultrasound, CT, MRI, and radiography detect metastases to other organs.
The final diagnosis is established based on the histological examination of tumor fragments. Due to the high risk of metastasis, aspiration biopsy is inadvisable. Usually, resection of the tumor through a small incision is performed. The removed tissues are sent for examination, and based on their results, a decision on further therapeutic and diagnostic actions is made.
Testicular cancer treatment
A comprehensive approach is used in the treatment of testicular cancer. To eliminate the primary tumor, surgery is performed to remove the affected genital gland. Surgery is supplemented with chemotherapy and radiation.
Conservative treatment
The need for radiotherapy and chemotherapy is determined on a personalized basis. Pharmacologic therapy with platinum-based drugs may be used before surgery. Radiation therapy is usually performed after surgery. After treatment is completed, hormone replacement therapy may be prescribed.
In inoperable forms of cancer, palliative therapy is performed to reduce the intensity of symptoms and improve the patient’s quality of life.
Surgical treatment
The standard of treatment for testicular cancer is surgery – orchofuniculectomy. The intervention involves removing the affected gland and the spermatic cord. In some cases, the operation is supplemented with lymphadenectomy, which contributes to achieving remission.
In bilateral lesions, it is possible to remove both testicles. To eliminate the cosmetic defect, testicular prosthetics with silicone implants are performed.
All these treatment options are available in more than 850 hospitals worldwide (https://doctor.global/results/diseases/testicular-cancer). For example, orchiectomy is performed in 13 clinics across Israel for an approximate price of $7.2 K (https://doctor.global/results/asia/israel/all-cities/all-specializations/procedures/orchiectomy).
Prevention
Preventive measures regarding testicular cancer in case of belonging to a high-risk group (cryptorchidism, unfavorable family history, testicular atrophy, etc.) imply regular monitoring of the state of the glands with the help of ultrasound. Generally, men should give up bad habits, lead an active lifestyle, and minimize contact with harmful substances.
Rehabilitation after surgical treatment
In the postoperative period, radiation, symptomatic therapy, and drug prevention of complications are usually performed. The timing and peculiarities of the recovery period depend on the scope of the intervention. Usually, patients are recommended to bathe in the shower instead of bathing and refrain from physical exertion and sexual activity. In the future, it is necessary to undergo regular control examinations.