Barrett’s esophagus
Overview
Barrett’s esophagus, or Barrett’s metaplasia, is a severe complication of reflux disease (GERD), which consists of pathological changes in the esophageal mucosa.
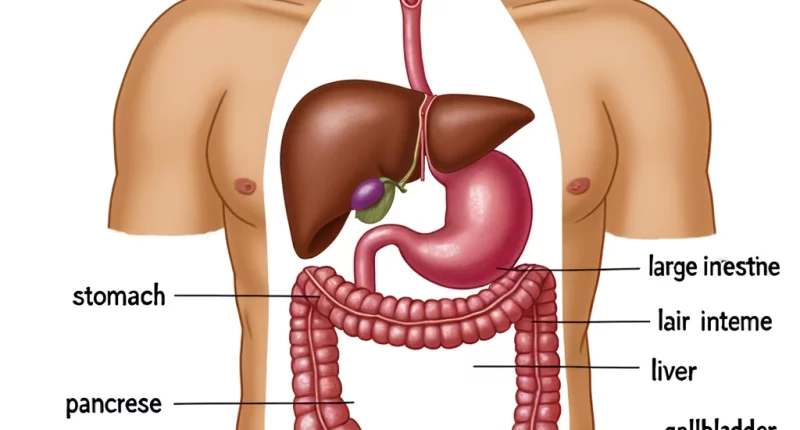
Prolonged exposure to acid and bile on the esophageal mucosa in gastroesophageal reflux disease leads to its chronic inflammation and erosive and ulcerative changes; without proper treatment begins the process of metaplasia – degeneration, and replacement of normal cells of the esophageal mucosa with cells characteristic of the intestinal mucosa.
A related disease, which often leads to the constant throwing of gastric contents into the esophagus, is a hernia of the esophageal opening of the diaphragm.
Symptoms of Barrett’s esophagus
- heartburn;
- Indigestion;
- Difficulty swallowing solid foods;
- bitterness in the mouth;
- Blood in vomit or stool;
- pain behind the sternum.
approximately 25% of cases are asymptomatic.
Complications of Barrett’s esophagus
The danger of this disease is that the degeneration of the intestinal mucosa cells is a single process that successively passes several stages with increasing severity of changes and, as a result, can lead to the development of a malignant tumor. In this regard, Barrett’s metaplasia is a precancerous condition. In almost half of cases, the initial metaplasia of esophageal mucosa cells leads to further abnormal development (dysplasia) and eventually transforms into a cancerous tumor – adenocarcinoma, the mortality rate of which reaches 90%.
Barrett’s metaplasia can develop in different parts of the esophagus; metaplasia in the area of the cardiac part of the stomach (located immediately after the transition of the esophagus into the stomach) can develop not only on the background of GERD, quite often, it develops on the background of gastritis in the presence of Helicobacter pylori.
In addition to reflux disease itself, an independent risk factor for the development of esophageal adenocarcinoma is obesity. The risk of developing adenocarcinoma is significantly increased in the presence of both factors.
Diagnosis of Barrett’s esophagus
To diagnose Barrett’s esophagus, a gastroscopy with multilevel biopsy of areas of altered esophageal mucosa is performed (a gastroenterologist performs the procedure). The diagnosis is established only after a histologic study confirms pathologic changes in the epithelium. Endoscopic examination and biopsy allow us to detect cell degeneration and determine the nature and degree of severity (metaplasia or dysplasia) and their localization. Treatment is prescribed depending on the severity of the existing changes in the esophageal mucosa.
Diagnosing Barrett’s esophagus can be challenging as this condition does not impact the entire esophageal tissue. The doctor extracts biopsy specimens from at least eight distinct regions of your esophagus’s lining to assess the condition.
Screening for Barrett’s esophagus
Your physician might advise screening for Barrett’s esophagus if you are a male experiencing chronic (persisting for over five years) and frequent (occurring weekly or more) GERD symptoms, along with possessing two or more risk factors associated with Barrett’s esophagus. These risk factors encompass:
- Being 50 years of age or older.
- Current or past smoking habits.
- Possessing a significant amount of abdominal fat.
- A family history of Barrett’s esophagus or esophageal adenocarcinoma.
Treatment of Barrett’s esophagus
Treatment of patients with Barrett’s esophagus is aimed at treating GERD, against which metaplasia has developed, and preventing the development of esophageal cancer.
The principles of treatment of Barrett’s metaplasia at the initial stage are the same as in the treatment of uncomplicated GERD; only the therapy should be more intensive. Patients with Barrett’s esophagus without dysplasia are recommended to undergo endoscopic examination once every 2-3 years. If histologic examination reveals low-grade dysplasia, treatment should be intensified, and the period of regular examinations should be reduced to six months.
Medicines
Treatment for Barrett’s esophagus and gastroesophageal reflux disease (GERD) often involves the use of acid-lowering medications known as proton pump inhibitors (PPIs). These drugs aid in preventing further harm to the esophagus and may even repair existing damage in some cases.PPIs available are:
Omeprazole;
Pantoprazole;
Rabeprazole;
Lansoprazole;
Esomeprazole;
Dexlansoprazole.
Endoscopic treatment
- If drug treatment is ineffective, radiofrequency ablation (RFA) is indicated for patients with Barrett’s esophagus. This is a minimally invasive endoscopic procedure based on the therapeutic effect of radiofrequency waves on the affected tissue. This procedure can quickly, safely, and effectively remove areas of metaplasia on the esophageal mucosa.
- Photodynamic therapy involves a light-sensitive chemical known as porfimer (Photofrin), an endoscope, and a laser to eliminate precancerous cells in the esophagus. In this treatment, a doctor administers porfimer via an injection into a vein in your arm. After 24 to 72 hours, you return to undergo the final steps of the procedure.
- Endoscopic mucosal resection is when the doctor elevates the Barrett’s tissue, either by injecting a solution beneath it or using suction and subsequently excising it. The tissue is then extracted using an endoscope. This technique is carried out by gastroenterologists in select hospitals and outpatient facilities. During the procedure, you’ll be given local anesthesia to numb your throat and a sedative for relaxation and comfort. Before conducting an endoscopic mucosal resection to treat cancer, an endoscopic ultrasound is performed by your doctor.
Surgical treatment
In radical surgical treatment of Barrett’s esophagus, the pathologically altered part of the esophagus is removed by transhiatal extirpation with one-stage plasty with a gastric tube. In the radical surgical treatment of Barrett’s esophagus, the pathologically altered part of the esophagus is removed by transhiatal extirpation with one-stage gastric tube plastic. The long-term results of radical operations performed for Barrett’s esophagus are more favorable than those for esophageal adenocarcinoma.
Barrett’s esophagus is treated in more than 590 hospitals around the world (https://doctor.global/results/diseases/diaphragmatic-hernia). For instance, a total esophagectomy, which involves the complete removal of the esophagus, can be performed at a clinic in the Netherlands, with costs ranging between 23822USD and 60092USD.(https://doctor.global/clinic/jeroen-bosch-ziekenhuis#prices).