Uterine cancer
What is it?
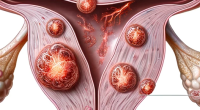
Uterine cancer, or adenocarcinoma of the uterus, is a malignant tumor that develops in the glandular epithelial cells. The cancer most often affects the body of the uterus, much less often occurs in the cervix. This type of cancer is a significant health concern for women worldwide. This malignancy, predominantly affecting the endometrium, the inner lining of the uterus, is characterized by the abnormal growth of glandular cells.
Treatment of this disease is performed by a gynecologist
About uterine cancer
Uterine adenocarcinoma usually develops in the body of uterus. The proportion of malignant glandular lesions in the cervix accounts for only 25% of cases.
The early stages of the disease may be asymptomatic. However, it is most often manifested by acyclic bloody discharge from the genitals. In women of childbearing age, they appear between periods. In patients past menopause, the appearance of spotting at any time is always suspicious of a malignant process. In this situation, in the first stage, an ultrasound is indicated.
It should be noted that in menopause, blood spots may be associated not only with a malignant process. Other causes include sudden rise in blood pressure, use of non-steroidal anti-inflammatory drugs, etc. An extended examination is performed to clarify the diagnosis.
Treatment of adenocarcinoma is determined by the stage of the pathological process. If the general condition of the woman allows, then treatment begins with radical surgical intervention. In addition, radiotherapy, hormone therapy or chemotherapy may be performed.
The prognosis for adenocarcinoma of the cervix and uterine body is determined by the stage of the disease, the localization of the tumor, the form of anatomical growth, the depth of invasion of the stroma, the presence of lymph node lesions and necrosis of the fields of cancer.
Causes and Risk Factors
Adenocarcinoma is usually sporadic. The development of the disease involves long-term exposure to causative factors that can alter the genetic makeup of the cell. In only 5% of cases, this is an inherited pathology caused by mutant genes that alter the typical structure of epithelial structures. Among familial forms, Lynch syndrome is the most common. This condition is characterized by the development of malignant tumors, not only in the uterus but also in the colon (the tumors are often multiple).
While the exact cause of uterine cancer is unknown, several risk factors have been identified:
- Age: The risk increases with age, particularly after menopause.
- Hormonal Imbalance: An imbalance of estrogen and progesterone, especially excess estrogen exposure without progesterone, can increase the risk.
- Obesity: High body fat can lead to increased estrogen levels, elevating the risk.
- Family History and Genetics: A family history of uterine or other types of cancer can increase risk. Specific genetic changes (like Lynch syndrome) are also risk factors.
- Using the anti-estrogenic drug Tamoxifen.
- Other Factors: These include nulliparity (never having given birth), early menstruation, late menopause, and certain types of hormone therapy after menopause.
Different forms
Adenocarcinoma of the uterus is divided into two groups:
- The first type. This is the most common variant, which develops with a background of atypical endometrial hyperplasia. Predisposing factors include diabetes, hypertension, and excess body fat. In other words, the first type of uterine adenocarcinoma is associated with metabolic syndrome. It most commonly affects patients between the ages of 45-50 years. The prognosis for uterine adenocarcinoma of the second type is more favorable because tumors of this type are characterized by high levels of cell differentiation.
- The second type. These tumors are commonly derived from atrophic endometrium. Pathogenetically, they are not associated with excess estrogen. Most often, they have low differentiation grade, so the prognosis is worse. Adenocarcinomas of the second type occur most commonly in women who are menopausal.
According to the histological structure, most malignant tumors of the uterine body include endometrial adenocarcinoma. Mixed adenocarcinomas may also occur.
According to the maturity of the cells in the tumor, three classes of adenocarcinomas are distinguished:
- high differentiation;
- moderate differentiation;
- low differentiation.
When making a clinical diagnosis, the oncogynecologist will consider the TNM classification, which is used to determine the extent of the prevalence of the malignant process. There are four stages of uterine adenocarcinoma:
- first stage – the tumor does not cross the epithelial layer of the uterus;
- the second stage – the cancer has spread beyond the basal lamina into the muscular layer;
- third stage – the tumor has spread outside the boundaries of the uterus; the tumor cells are found in the lymph nodes of the small pelvis;
- the fourth stage – is distant metastases, which indicate the spread of a malignant process in the body.
Symptoms of uterine cancer
Adenocarcinoma of the uterus is associated with the presence of a bloody discharge. In women with preserved menstrual function, they appear on intermenstrual days and are not cyclic. If the patient is menopausal, then the first discharge may be a slight bleeding from the genitals. It may be spontaneous or provoked by sexual intercourse. Meanwhile, in clinical practice, asymptomatic cases of adenocarcinomas are often found, which have been detected on a contraceptive ultrasound examination.
Diagnostics
Indirect signs of uterine adenocarcinoma are most often detected by ultrasound. They may include an increase in the thickness of the endometrium, the appearance of pathological inclusions, fluid in the uterine cavity, and a change like the vascularization of the endometrial blood vessels. In menopause, an essential diagnostic criterion is the thickness of the endometrium. It is considered that if the duration of menopause is five years or more, the endometrial thickness is 4 mm or less. In this case, the probability of a malignant process does not exceed 5%.
The final diagnosis is confirmed based on the results of the morphological examination. The material is obtained by a separate diagnostic scraping under the supervision of a hysteroscopy. In some cases, as an option, it is possible to perform an aspiration biopsy of the endometrium when a negative pressure zone is created using a syringe or special probe that promotes “separation” of the biomaterial.
A colposcopic examination (simple and extended sampling) is helpful to detect cervical adenocarcinoma. For the most suspicious spots and ectocervix (the outer surface of the cervix), the material is obtained by “pinching.” To examine the tissue structure of the exocervix (cervical mucosa), a diagnostic scraping of the cervical canal is performed.
The following methods are also included in the study program for patients with suspected adenocarcinoma:
- a general clinical blood test;
- biochemical blood tests;
- cancer markers CA-125, CA 19-9;
- evaluation of blood clotting activity;
- general clinical urine analysis;
- ultrasound of the abdominal organs;
- chest X-Ray;
- computed tomography with contrast or positron emission tomography (to assess the condition of the lymph nodes).
Treatment of uterine adenocarcinoma
Surgery for uterine adenocarcinoma is a crucial treatment option that, depending on the stage, can be isolated or combined with other methods. If, for health reasons, surgical intervention is contraindicated, then medical treatment begins with radiotherapy.
Conservative treatment
The conservative treatment option is determined by the malignant process’ prevalence and the tumor’s characteristics. In modern oncogynecology, there is a large arsenal of possibilities.
- If the adenocarcinoma of the uterus has a high degree of differentiation, it is possible to do targeted hormone therapy. This treatment option is justified for endometrial cancer that has receptors for steroid hormones.
- Depending on the stage of the malignant process after surgery, radiotherapy may be necessary – intracavitary or remote.
- If the tumor process is widespread, chemotherapy may be included in a comprehensive treatment program.
Surgical treatment
The scope of the surgery is to remove the body and cervix of uterus, appendages (ovaries and fallopian tubes), along with the affected lymph nodes. For young women who intend to give birth in the early stages of a malignant process (if it has not gone beyond the basal lamina of the epithelium), organ-preserving surgery is possible. However, such tactics require a detailed discussion with a medical consultation involving specialized experts with experience managing such patients.
This disease can be treated with vaginal hysterectomy, which is performed by the 731 hospital worldwide (https://doctor.global/results/diseases/endometrial-cancer/procedures/vaginal-hysterectomy) with the average cost of $18.3 K. In Germany this procedure is performed in 32 clinics with average price of $13.3 K (https://doctor.global/results/europe/germany/all-cities/all-specializations/procedures/vaginal-hysterectomy)
Prevention
Specific measures for the prevention of uterine adenocarcinoma have yet to be developed. To reduce the risk of a malignant process, you should follow the following rules:
- keep track of your weight and avoid becoming obese.
- maintain adequate physical activity (at least 150 minutes per week).
- increase the proportion of coarse fiber in the diet;
- in the presence of diabetes mellitus – to maintain adequate carbohydrate metabolism.
Rehabilitation services
Patients after surgical treatment of uterine adenocarcinoma are advised to follow the following rules:
- if possible, start early with activation – beginning with a movement around the ward so the activity level is gradually expanded.
- regularly change bandages – at the beginning of the hospital, after discharge – at a follow-up appointment with an oncogynecologist;
- expand the diet progressively – on the first day, it must contain only non-carbonated tap water (you can add a slice of lemon); from the second or third day, liquid food, then switch to pureed food and then the usual.
All patients who underwent surgery for adenocarcinoma of the body or cervix must be registered with a medical center that has an oncogynecologist. Preventive checks are prescribed at a specific frequency to identify possible recurrence and timely carry out targeted treatment.
A routine physical examination program usually includes the following tests:
- gynecological examination;
- taking cytological smears of the stump of the vagina;
- ultrasound scanning of the abdominal cavity and peritoneal space;
- X-Ray examination of the thoracic organs;
- evaluation of cancer markers CA-125 and others according to the indications;
- computer or nuclear magnetic tomography.
Conclusion
Uterine adenocarcinoma, while a challenging diagnosis, has seen significant advancements in detection, treatment, and care. Understanding the disease, recognizing the symptoms, and accessing timely medical care are critical steps in combating this cancer. Through a combination of advanced medical treatments and supportive care, many women with uterine adenocarcinoma continue to lead fulfilling lives.