Uterine fibroids
What is it?
Uterine fibroid, or uterine leiomyoma, is a type of benign tumor in which myomatous nodules are composed of smooth muscle cells (unlike fibroma, which is represented by dense fibrous tissue).
About the disease
Leiomyomas of the uterine body occur in 95% of cases, and only in 5% of cases the tumor is located in the cervix. The disease is insidious with its complications. Against the background of heavy menstruation, the risk of anemia increases, which in some women is severe. The presence of uterine deformities can negatively affect the possibility of conception.
Uterine leiomyoma can also be the cause of acute conditions. The pedicles of the subserosal nodes can twist, leading to the “acute abdomen” clinic. In this case, the woman is bothered by intense pain in the lower abdomen, which leads to reflex tension of the muscles of the anterior wall. There may even be an increase in body temperature. A similar picture develops with ischemia of the myomatous node when its blood supply is disturbed. Submucosal nodes can occur, which is manifested by bloody discharge and intense contraction-like pain in the lower abdomen.
The risk of malignant transformation of pathological foci in uterine fibroids is very low – no more than 1%. However, this tumor still retains oncological vigilance. It is primarily due to the imbalance of sex hormones. It increases the risk of developing atypical hyperplasia of the endometrium and, accordingly, endometrial cancer.
Types
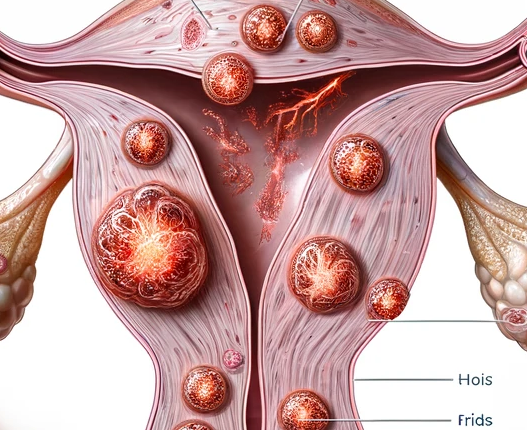
Uterine leiomyomas are divided into the following varieties according to the nature of myomatous node growth:
- interstitial – the pathologic zone is located in the intermuscular layer;
- subserosal – the nodule grows towards the abdominal cavity and may be found on a wide base or on a thin pedicle;
- submucosal – the pathologic zone deforms the uterine cavity;
- intraligamentary – the nodes grow between the layers of the uterine ligamentous apparatus.
This classification describes the nature of nodal growth in general terms and does not always provide comprehensive information regarding the management of the patient. Therefore, the international organization FIGO has significantly supplemented it by identifying eight types of uterine leiomyoma.
Myomatous nodes can be small or large. The latter variant is said to be more than 5 cm in diameter.
Symptoms of uterine leiomyoma
For a long time, uterine leiomyoma may not manifest itself in any way, and a woman, as a rule, first learns about the presence of the disease during a routine gynecological examination.
However, in 1/3 of patients, symptoms are present almost immediately. The main manifestations of the disease are:
- menstrual disorders – heavy and prolonged menstruation;
- intermenstrual bleeding;
- lower abdominal pain;
- dysfunction of pelvic organs (bladder, rectum) – frequent urination, urinary retention, difficulty in defecation;
- infertility, in the development of which plays a role in the nodes that deform the uterine cavity.
Causes of uterine fibroids
Today, risk factors that increase the likelihood of developing this disease have been identified. These include:
- early onset of menstruation (at 9-10 years of age);
- no history of childbirth;
- age over 40;
- obesity;
- being a member of the negroid race;
- taking phytoestrogens and medications for menopausal hormone therapy;
- genetic breakdowns;
- painful menstruation.
During prolonged experiments, a protective factor has also been discovered. It is adequate physical activity which reduces the risks of uterine myoma development.
It is believed that the mechanism of benign hyperplasia in uterine myoma is related to the hypersensitivity of the myometrium to sex hormones. In such women, the blood content of both estrogen and progesterone fractions is increased. At the same time, the number of receptors to these hormones is also increased, and accelerated conversion of testosterone into estrogens is noted.
These changes increase the activity of cell division and increase the risk of mutations in cells. Progesterone makes the uterine muscular layer tissues more sensitive to growth factors and less susceptible to factors of programmed cell death. The result is the formation of myomatous nodules sooner or later.
Diagnosis
Diagnosis of uterine leiomyoma is not very difficult. The initial assumption of the presence of this benign tumor arises at the stage of bimanual examination when an increase in the size of the uterus and deformation of its external contour is detected.
An ultrasound scan of the pelvic organs is performed to confirm the diagnosis. And both transabdominal and transvaginal access. In some cases, to visualize the uterine cavity through the cervical canal can be injected with fluid (echohysterosonography). This method helps to distinguish submucosal nodules from endometrial polyps.
The examination may be supplemented by hysteroscopy if indicated. It assesses the uterine cavity using endoscopic equipment inserted into the uterine cavity through the cervical canal. Diagnostic hysteroscopy can turn into therapeutic hysteroscopy if submucosal myomatous nodes or polyps are found. Scraping of the uterine cavity is performed if there is a suspicion of endometrial pathology since only morphological examination helps to exclude atypical and malignant transformation of cells definitively.
Treatment of uterine leiomyoma
The choice of treatment tactics for patients with uterine leiomyoma depends on several factors. First, the nature of the symptoms. Second, the size of the tumor. Thirdly, reproductive plans. A wait-and-see tactic is chosen for an asymptomatic course of small neoplasms. After the onset of menopause, regression of the pathologic site is observed, with maximum expression in the first 5-7 years of persistent cessation of ovarian function.
Myomas that result in abnormal uterine bleeding, pelvic organ dysfunction, chronic pain or infertility, and masses of significant size should be treated.
Conservative treatment
Drug therapy can be symptomatic and pathogenetic. The first option is aimed at controlling pain (non-steroidal anti-inflammatory drugs are used) and stopping uterine bleeding (tranexamic acid and analogs). The second option, by stabilizing the level of hormones, reduces the size of myomatous nodes and prevents heavy menstruation and the appearance of intermenstrual bloody discharge.
The following groups of drugs may be used as part of pathogenetic therapy:
- Progestogens. These include intrauterine contraceptives in which the active substance is levonorgestrel. The spiral is installed for several years; there is a constant release of progestogen. Over time, it causes atrophy of the endometrium, resulting in menstruation becoming scanty, sometimes barely smearing. At the same time, the size of the nodes also decreases.
- They combined hormonal contraceptives. These drugs affect only menstrual function (reduce the volume of blood lost) but do not act on the myoma. Some representatives of this class can even stimulate the pathological growth of the node.
- Gonadotropic hormone antagonists. They cause a state of artificial menopause. On the one hand, it positively affects myoma (blocks its growth). Still, on the other hand, it can lead to the development of menopausal manifestations and estrogen deficiency. The latter circumstance limits the active use of this class of substances. The course of treatment can last up to six months.
- Selective progesterone receptor modulators. They cause a state of medically induced cessation of menstruation and reduce the size of the nodes. However, after withdrawal, resumption of pathologic growth is not excluded.
Operative treatment
There are several surgical options for this condition.
- Myomectomy. Surgical removal of fibroids, preserving the uterus.
- Hysterectomy. Removal of the uterus, completely eliminating the possibility of fibroid recurrence.
- Endometrial Ablation. Destroys the lining of the uterus. It can reduce bleeding but doesn’t eliminate fibroids.
- Uterine Fibroid Embolization (UFE). A minimally invasive procedure that cuts off blood supply to fibroids, causing them to shrink.
All these surgical treatment options are performed in more than 800 hospitals worldwide (https://doctor.global/results/diseases/uterine-fibroids). For example, Laparoscopic myomectomy is performed in 32 clinics across Germany for an approximate price of $13.2 K (https://doctor.global/results/europe/germany/all-cities/all-specializations/procedures/laparascopic-myomectomy).
Prevention
No specific preventive measures have been developed. Taking into account risk factors, it is recommended to reduce the probability of myoma development:
- birth of the first child under the age of 30;
- abortion denial;
- taking hormonal contraceptives;
- weight control;
- an adequate level of physical activity.
Rehabilitation after surgical treatment
The recovery period after surgery lasts 2 to 4 weeks, depending on the technique and extent of surgery. Several restrictions should be observed until the tissues are completely healed:
- do not lift weights over 5 kilograms;
- eliminate sexual intercourse;
- Do not take a hot bath or go to a sauna.
The attending obstetrician-gynecologist will inform the patient about removing restrictions and possibly returning to the usual way of life.