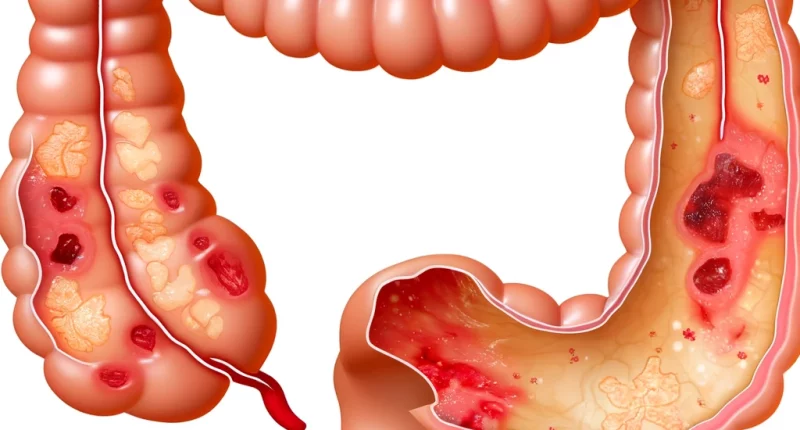
Ulcerative colitis
What’s that?
Ulcerative colitis is an inflammatory disease of the mucosa of the large intestine, which has a severe chronic character. The cause of pathology development is a combination of several factors at once, which include hereditary, external (infections, nutrition, lifestyle), and internal (state of organs, immune system) factors.
About the disease
The most frequent cases of colitis are found in developed European and North American countries. The prevalence of the disease in Europe is 20-30 cases per 100 thousand population. The pathology most often occurs in men and women aged 20 to 42 years, as well as in older people.
Ulcerative colitis can have two of the most dangerous periods of development:
- The first year; during this time, the likelihood of developing life-threatening complications is high;
- The tenth year, the likelihood of malignant neoplasms increases by this point.
Types of ulcerative colitis
The European Consensus on the Diagnosis and Treatment of Ulcerative Colitis in 2006 distinguished three forms of the disease according to the extent of the disease:
- Proctitis – the inflammatory process occurs only in the rectum and is limited to the rectosigmoid angle;
- Left-sided colitis – inflammation reaches the splenic flexure of the colon;
- Disseminated colitis is a complete lesion of the large intestine.
Depending on the severity of the course of the pathology, three degrees are distinguished:
- light;
- mild;
- severe.
Classification of ulcerative colitis according to the nature of development and course:
- Acute: less than six months have passed since the first manifestation of the disease;
- A fulminant (rapidly developing) course;
- Chronic continuous course: with adequate treatment, remission periods are less than six months;
- Chronic recurrent course: periods of remission lasting more than six months.
In the recurrent course of the disease, rarely recurrent (less than once a year) and frequently recurrent (2 times a year or more) are distinguished. Exacerbations of ulcerative colitis, as a rule, occur as a result of improper diet, stress, or taking certain medications but can occur without an apparent reason.
Symptoms of ulcerative colitis.
Ulcerative colitis is characterized by a cyclic course: periods of remission alternate with exacerbations. During remissions, signs of NSAIDs are usually absent, while exacerbations are characterized by various manifestations that vary depending on the localization of inflammation and the intensity of the course of the disease.
The main symptoms of proctitis are:
- lower abdominal pain;
- bloody discharge from the anus;
- painful urges to empty the bowels.
Signs of left-sided ulcerative colitis involving the descending colon are:
- bloody diarrhea;
- weight loss;
- pronounced pain in the left side of the abdomen.
Disseminated ulcerative colitis with total colonic involvement is characterized by:
- constant abdominal pain;
- persistent, profuse diarrhea accompanied by bleeding.
In the latter case, the patient’s life is threatened by severe dehydration and blood loss.
It is also noted that sometimes people with ulcerative colitis may have symptoms other than bowel symptoms:
- stomatitis;
- vascular inflammation;
- joint disease;
- dermatologic pathologies;
- biliary tract disease;
- bone softening or osteoporosis;
- ocular inflammatory diseases.
Causes of ulcerative colitis
At the moment, the causes of the disease remain unclear. It is statistically determined that ulcerative colitis of the intestine is more often diagnosed in people whose relatives had this pathology, and therefore, the leading cause is considered to be genetic predisposition. The key to the development of ulcerative colitis is believed to be an imbalance of the immune system. The pathogenic microorganism provokes an immune response, due to which an inflammatory process develops, affecting the intestinal mucosa and leading to ulcers and erosions.
There are several significant factors in the development of ulcerative colitis:
- long-term antibiotic use;
- viral and bacterial infections;
- hereditary predisposition;
- congenital and acquired immune defects.
Diagnosis of ulcerative colitis
A proctologist carries out the diagnosis and treatment of pathology. First of all, the specialist collects complaints and anamnesis and then examines the patient, including a finger examination of the rectum.
For further investigation and differentiation from Crohn’s disease and other diseases of similar type, a comprehensive diagnostic examination of the patient is required. The most important procedures are colonoscopy with intestinal biopsy and sigmoidoscopy. These methods allow visual assessment of the condition of the mucosa of the colon.
To clarify the presence of edema, perforations, ulcers, and other formations (inflammatory polyps, thickenings, etc.), a radiologic study may be prescribed.
In addition to instrumental methods, laboratory diagnostics is performed:
- general blood test to detect leukocytosis and anemia;
- stool analysis to determine the severity of the inflammation process;
- biochemical blood test to exclude concomitant pathologies;
- A and B clostridium toxin fecal examination to rule out clostridial intestinal infection.
Treatment of ulcerative colitis
The therapy depends on the degree of intestinal damage and the severity of the disease. If only the rectum is affected, then outpatient treatment is usually sufficient. In left-sided and widespread colitis, hospitalization is necessary.
Treatment for ulcerative colitis includes diet, drug therapy, and, if necessary, surgery.
Conservative treatment
The main purpose of drug therapy is to control the symptoms of the disease and stop the development of inflammation and ulceration.
In ulcerative colitis, the doctor prescribes several groups of medicines:
- painkillers;
- anti-diarrheal;
- immunosuppressants;
- iron supplements for anemia;
- nonsteroidal and hormonal anti-inflammatory drugs.
Diet plays a vital role in the process of therapy. The patient is forbidden to eat fiber-rich food and fried, fatty, spicy, salty, and acidic dishes. At the same time, it is recommended to eat more protein products.
In the period of severe exacerbation, a complete refusal of food may be recommended to facilitate the work of the intestines. In this case, nutrients are administered intravenously.
Surgical treatment
If conservative therapies are ineffective, surgeons excise the affected part of the colon. After that, a reservoir is formed from a section of the small intestine to take over the functions of the removed section. If the size of the lesion is small, the use of a transplant is not necessary.
All these treatment options are available in more than 770 hospitals worldwide (https://doctor.global/results/diseases/ulcerative-colitis). For example, sigmoidectomy can be performed in 25 clinics across Turkey for an approximate price of $7.4 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/sigmoidectomy).
Prevention of ulcerative colitis
Since the causes of ulcerative colitis have not been thoroughly investigated, the primary preventive measure is to maintain a healthy lifestyle:
- minimizing stressful situations;
- adherence to a proper diet;
- quitting smoking and alcohol abuse;
- maintaining moderate physical activity.
Rehabilitation
After surgery, the patient can return to everyday life in 2-3 weeks. In severe complications, it may take up to four months to regain total capacity. After discharge from the hospital, the patient should follow the attending physician’s instructions and get on the dispensary register. Until the healing of tissues, it is necessary to limit physical activity, carrying heavy weights, heat procedures, and insolation. To maintain a normal state of health, annual sanatorium-resort treatment is recommended. Diet is prescribed for life.