Abnormal Uterine Bleeding
Abnormal uterine bleeding (AUB) is the discharge of blood from the organs of the female reproductive system. Bleeding can be juvenile (during puberty), menopausal (at the stage of reproductive function decline), and can also occur in women of childbearing age.
The pathogenesis of dysfunctional uterine bleeding is based on disorders of neuroendocrine control of synthesis and secretion of gonadoliberin by the hypothalamus, arising under various environmental factors. As a result, ovarian functionis disturbed, and hyperestrogenism develops, accompanied by hyperplastic processes in the endometrium, which become the substrate of uterine bleeding.
The probability of developing this pathology increases with age and decreases with each childbirth and lactation period. In most cases, dysfunctional uterine bleeding is not life-threatening.
Nevertheless, it is a highly unpleasant condition that leads to the deterioration of a woman’s well-being, mood, and appearance and limits her sexual, social, and physical activity.
Diseases
Uterine bleeding can be a symptom of various diseases of the female reproductive system.
- Uterine adenocarcinoma
- Uterine adenomyosis
- Hyperprolactinemia
- Hyperestrogenism
- Hypothyroidism
- Uterine myoma
- Cervical polyp
- Endometrial polyp
- Cervical cancer
- Endometriosis
- Cervical erosion
Diagnosis of uterine bleeding
It is essential to keep a cycle calendar, which will help you avoid the beginning of the cycle failure and take the necessary measures to eliminate it in time. In case of more prolonged than usual menstruation, lower abdominal pain, as well as blood clots from the external genital tract, should immediately consult a specialist.
The doctor collects a gynecological and obstetric history, learns about the medications taken, performs a physical examination, measures blood pressure and pulse, and records other body parameters that can be found without using instruments. The specialist then examines the cervix in mirrors and performs a bimanual vaginal examination.
The following tests may be ordered to find out the causes.
- Blood and urine tests, tests to determine hormone levels, gynecological smears, and tests for infections.
- Ultrasound of the pelvic organs. Ultrasound assesses the state of the endometrium (uterine mucosa), myometrium (uterine muscular layer), ovaries, fallopian tubes, and cervix. It allows the detection of polyps, tissue overgrowths, and other pathologies.
- Magnetic resonance imaging (MRI) of the pelvic organs. It allows you to get detailed information about the state of tissues of different densities. It is used when ultrasound is not sufficiently informative.
- Colposcopy. Examination of the vagina and cervix using a colposcope, which allows visualization with multiple magnification. Various tests are performed simultaneously, and a biopsy may be taken.
- Hysteroscopy. Examination of the uterus from the inside using a hysteroscope (a probe with optics and illumination) The technique is performed in case of suspected endometrial polyp, uterine myoma, i.e., focal pathology.
- Tissue biopsy. Taking a tissue sample allows the cellular structure of the altered area to be assessed.
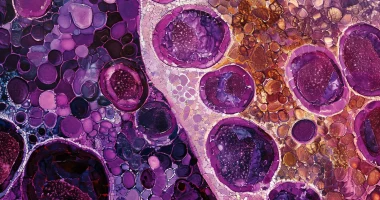
- Separate diagnostic curettage. The inner layer of the uterus and cervical canal is scraped off using a special curette (a loop with sharp edges). Subsequently, a histologic examination is performed under a microscope.
If necessary, other tests may be prescribed for a more accurate diagnosis.
Which doctor to see
In case of heavy menstrual and intermenstrual bleeding and prolonged and profuse bloody discharge, it is necessary to consult a gynecologist. Then, the doctor can treat the patient independently or refer to colleagues of other specialties.
Types of uterine bleeding
The classification of uterine bleeding was developed to streamline and standardize the different types of pathology. Currently, gynecologists use the 2011 PALM-COEIN classification for abnormal uterine bleeding in non-pregnant women of reproductive age.
The acronym PALM-COEIN consists of two parts: PALM and COEIN. These letters represent the main groups of causes of uterine bleeding.
PALM:
- P (Polyp). Polyps are benign growths of the uterine mucosa, i.e., the endometrium.
- A (Adenomyosis). It is a condition in which the epithelium of the inner lining of the uterus (endometrium) grows into the myometrium (the muscle layer of the uterus). Adenomyosis can cause painful and/or heavy bleeding.
- L (Leiomyoma). It is a benign tumor consisting of smooth muscle tissue. Because the endometrium does not have the same surface, parts of the mucous layer are contracted at different times. Thus, some parts are rejected during menstruation, while others are rejected at other times, so a woman experiences acyclic bleeding.
- M (Malignancy and Hyperplasia) includes both benign and malignant tumors and hyperplasia, a precancerous condition of the endometrium.
COEIN:
- C (Coagulopathy) – a condition accompanied by abnormalities in hemostasis, i.e., the process of stopping bleeding. It can be caused by medications or hereditary pathology (e.g., Willebrand’s disease).
- O (Ovulatory Dysfunction) is a condition in which ovulation does not occur regularly or at all. Ovulatory dysfunction can lead to irregular and heavy uterine bleeding. Ovulatory disorders are more common during puberty and menopause.
- E (Endometrial) – localized dysregulation of bleeding-stopping mechanisms in the endometrium (e.g., endometritis).
- I (Iatrogenic) – bleeding caused by medical interventions and treatments. Direct effects on the endometrium, effects on coagulation (clotting), and systemic effects on ovulation can cause abnormal uterine bleeding. For example, the use of antibiotics and anticonvulsants that have an indirect impact on sex hormone levels in the body are sometimes iatrogenic causes of bleeding.
- N (Not Yet Classified). Pathologic changes that cannot be assigned to any of the existing categories of the classification system.
The PALM-COEIN system is essential for identifying and classifying the causes of uterine bleeding. It allows doctors to thoroughly examine the woman and then choose the appropriate treatment methods.
Causes of uterine bleeding
The causes of uterine bleeding can be related to various diseases and conditions:
- Polycystic ovary syndrome is a disease characterized by the formation of cysts in places where follicles were previously located.
- Primary ovarian insufficiency – irregular release of eggs by the ovaries and low production of sex hormones despite high levels of circulating gonadotropins.
- Hypothyroidism.
- Iatrogenic interventions, such as the use of hormonal contraceptives.
- Coagulopathies are diseases of blood clotting.
- Endometritis is an endometrium inflammation (the uterine cavity’s inner lining).
- Endometrial and cervical polyps – benign neoplasms formed on the mucous membrane of the canal of the cervix or body of the uterus, capable of malignancy.
- Adenomyosis.
- Leiomyoma.
- Cancer of the uterine body or cervix.
- Hyperprolactinemia is a condition characterized by an increase in the pituitary hormone prolactin in the blood.
- Periods accompanied by changes in hormone levels and menstrual cycle (puberty, menopause).
Treatment for uterine bleeding
To understand the causes of pathology and how to treat uterine bleeding, it is necessary to consult a specialist as soon as possible. The doctor will prescribe the required examination and determine a treatment plan aimed at managing the problem and eliminating its causes.
If the bleeding is heavy and cannot be stopped, the woman needs emergency treatment. If the bleeding is severe and cannot be stopped, the woman needs emergency treatment.
If the cause of discharge is a hormonal disorder, appropriate drugs are prescribed to normalize the work of endocrine organs. If bleeding is a consequence of taking any medication, it is canceled. After helping and stopping the bleeding, drugs to normalize the cycle are usually prescribed.
Methods of stopping bleeding:
- medication to stop the bleeding;
- surgical – cryodestruction, uterine scraping, endometrial ablation;
- uterine artery embolization.
Surgical intervention is indicated if drug treatment has failed.
Important: Self-medication in uterine bleeding is inadmissible and can lead to the development of several complications, up to death from blood loss.
All these surgical procedures are performed in more than 750 hospitals worldwide (https://doctor.global/results/diseases/abnormal-uterine-bleeding-aub). For example, uterine artery embolization is done in 8 clinics across Turkey for an approximate price of $4.3 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/uterine-artery-embolization-uae).
Complications
Complications of uterine bleeding are based on significantly prolonged blood loss. They may include:
- Iron deficiency anemia and associated dizziness, fainting, and weakness;
- Infertility (if hormonal failures cause abnormal uterine bleeding).
Hypovolemic shock: a life-threatening condition caused by a decrease in the amount of circulating blood. Without medical attention, it leads to a critical reduction in blood pressure and oxygen supply to the tissues. The result is fatal.
The consequences of uterine bleeding can be prevented by regularly visiting a gynecologist and seeking medical help promptly when any negative symptoms appear.