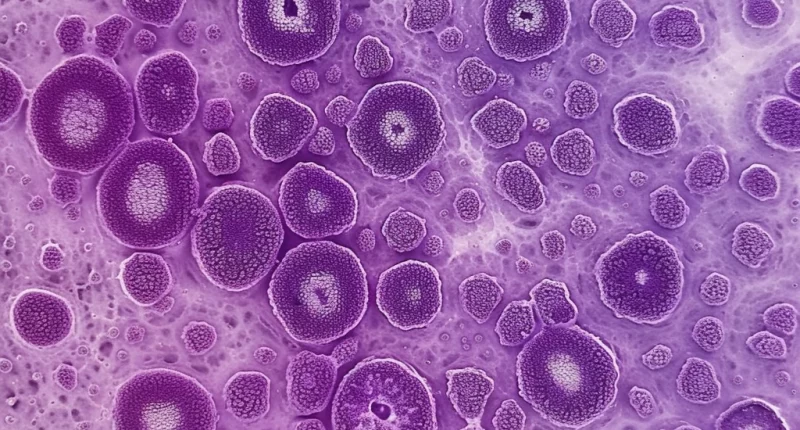
Cavernous hemangioma
What’s that?
Cavernous hemangioma is a benign tumor comprising clusters of small vascular cavities filled with blood. They can be located in different organs, but the most common variant is hemangioma of the liver, which will be discussed below.
5% of the adult population has this diagnosis. These neoplasms are more common in adults than in children: the typical age of patients is 30-50 years. Hemangiomas of the liver are more common in women than in men.
About the disease
Most liver hemangiomas do not cause symptoms, although larger masses that press on the tissue can cause poor appetite, nausea, and vomiting.
Usually, a patient develops only one hemangioma, but there may be several in some cases. Hemangiomas do not develop into cancer and do not spread to other parts of the body.
Classification of hemangiomas
There are several types of classification of hepatic hemangiomas, each of which is important in the selection of treatment:
1. Depending on the number of masses: single and multiple.
2. Depending on size:
- small: up to 15 mm in diameter;
- medium: 15-50 mm;
- large: more than 50 mm;
- giant: over 100 millimeters;
3. Depending on the internal structure: capillary (consisting of small cavities), cavernous (consisting of large cavities – caverns).
Symptoms of hemangioma of the liver
Most hemangiomas of the liver present without any signs and are discovered when the patient is seen for symptoms of another disease.
Giant hemangiomas of the liver (more than 10 cm) usually have symptoms that require treatment. Symptoms most commonly include pain in the upper abdomen as the large mass presses on surrounding tissue and the liver capsule. Other symptoms include:
- poor appetite;
- nausea;
- vomiting;
- a quick feeling of satiety during meals;
- a feeling of bloating after eating.
A liver hemangioma may bleed or form blood clots that retain fluid; that is why abdominal pain occurs.
Causes of hepatic hemangioma in adults
It is not reliably known why tumors arise in a particular organ. However, separate studies show that certain defective genes may cause liver hemangioma formation in men and women. There are suggestions that a role in the development of the tumor may play:
- long-term steroid therapy;
- long-term use of birth control pills;
- pregnancy.
Diagnosis of hepatic hemangioma
In most cases, hemangioma is an incidental finding that is discovered during ultrasound, CT or MRI of the abdominal cavity. The patient is referred to a hepatologist, who prescribes tests to determine the nature of the neoplasm:
- contrast-enhanced ultrasound – high-frequency sound waves are passed through body tissue, and echo signals are recorded and converted to video or photos;
- computed tomography (CT) scan;
- magnetic resonance imaging (MRI);
- angiography – a contrast agent is injected into the blood vessels to look at them when X-rays are taken;
- scintigraphy is a nuclear scan that uses the radioactive isotope technetium-99m to form an image of the hemangioma.
Additionally, general blood and urine tests, blood chemistry (various fractions of bilirubin and triglycerides, AST, ALT, and other tests), and consultations with specialists of related profiles may be prescribed.
Treatment
Some hemangiomas are diagnosed at birth or in early childhood (up to 5 – 10% of one-year-old children). The hemangioma usually shrinks over time and, in some cases, may disappear. If it is small, stable and does not cause any symptoms, it can be monitored with imaging studies every 6 – 12 months.
There are no medicines to treat hemangioma of the liver. Surgery may be needed to remove the tumor – if it is growing rapidly or causing significant discomfort or pain. A technique called vascular embolization, in which the blood vessels feeding the hemangioma are blocked can slow or reverse its growth. Sclerosing is very popular. This technique involves injecting a substance into the cavity of the mass that glues its walls together and prevents the tumor from forming again.
If this technique proves ineffective, surgical intervention is prescribed:
- segmental liver resection;
- removal of a lobe of the liver (lobectomy);
- removal of half of the liver (hemihepatectomy).
The choice of method of surgical treatment of hepatic hemangioma in men and women depends on the rate of its growth, severity of symptoms, and presence or absence of complications. Direct indications for surgery are:
- over 5 centimeters in diameter;
- tumor growth of 50% or more within a year;
- tumor rupture;
- symptoms of compression of surrounding tissues;
- suspicion of the malignant nature of the neoplasm.
All these treatment options are available in more than 600 hospitals worldwide (https://doctor.global/results/diseases/cavernous-hemangioma). For example, cavernous malformation treatment can be done in 28 clinics across Turkey for an approximate price of $10.5 K (https://doctor.global/results/asia/turkey/all-cities/all-specializations/procedures/cavernous-malformation-treatment).
Prevention
There is no specific prevention of the disease. Since the possible risk factors include taking several drugs, people taking steroids or oral contraceptives should undergo regular liver ultrasound to detect the mass in time.
Rehabilitation
Rehabilitation after treatment depends on the type of intervention. After embolization or sclerosing of the tumor, the patient returns to the usual rhythm of life in 1-2 weeks. When a part of the liver is removed, rehabilitation can be delayed for 1-3 months. During this period, it is necessary to limit physical activity and avoid fatty, fried and smoked foods and alcoholic beverages. In the first weeks after the intervention, it is also necessary to avoid overheating (including hot baths and saunas) and the open sunlight. The attending physician will make a schedule, which will help to keep the healing process under control.