Hepatic failure
Definition
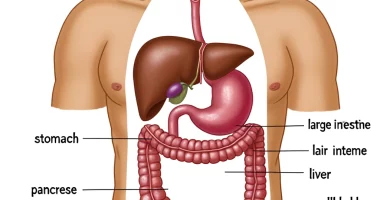
Hepatic failure is an acute or chronic syndrome that develops when one or more liver functions are impaired, accompanied by metabolic disorders, intoxication, CNS disorders, and the development of hepatic coma. The disease proceeds with the phenomena of hepatic cellular insufficiency (jaundice, hemorrhagic, dyspeptic, edema-ascetic syndromes, fever, weight loss) and hepatic encephalopathy (emotional lability, apathy, speech disorders, hand tremor, ataxia). The extreme degree of liver failure is the development of hepatic coma. Liver failure is detected based on biochemical indicators of blood, EEG, and hepatic scintigraphy. Treatment of liver failure is aimed at eliminating intoxication, normalization of electrolyte disorders, and restoration of acid-base balance.
General information
Liver failure develops with massive dystrophic, fibrotic, or necrotic changes in the liver parenchyma of various etiologies. Gastroenterology and hepatology distinguish acute and chronic course of liver failure. The leading pathogenetic link of liver failure is a violation of the detoxification function of the organ, in connection with which toxic metabolic products (ammonia, γ-aminobutyric acid, phenols, mercaptan, fatty acids, etc.) cause damage to the CNS. The development of electrolyte disorders (hypokalemia) and metabolic acidosis is characteristic. Lethality in liver failure reaches 50-80%.
Classification of liver failure
According to the clinical course, acute and chronic liver failure are distinguished. The development of acute liver failure occurs no later than two months after liver damage. Most often, the cause of acute failure is fulminant forms of viral hepatitis, alcoholic, drug, or other toxic liver damage. Chronic liver failure is caused by the progression of chronic liver disease (tumors, fibrosis, cirrhosis, etc.).
Four stages are distinguished in the development of liver failure: initial (compensated), severe (decompensated), terminal dystrophic, and hepatic coma. Hepatic coma also unfolds sequentially and includes the phases of precoma, threatening coma, and clinically expressed coma.
Causes of liver failure
Viruses, bacteria, and parasites play a leading role in liver failure. The most common cause of liver failure is viral hepatitis: hepatitis B (47% of cases), hepatitis A (5%), hepatitis C, D and E. On the background of viral hepatitis, liver failure more often develops in patients over 40 years old, with liver disease and alcohol and drug abuse. Less often, liver failure is associated with infection with Epstein-Barr virus, herpes simplex virus, adenovirus, cytomegalovirus, and others.
The following most frequent etiologic factors of liver failure are drugs and toxins. Thus, massive damage to the hepatic parenchyma can cause an overdose of paracetamol, analgesics, sedatives, or diuretics. The strongest toxins that cause hepatic failure are the poison of pale grebes, the mycotoxin of Aspergillus fungi, and chemical compounds (carbon tetrachloride, yellow phosphorus, etc.).
In some cases, liver failure may be due to hypoperfusion of the liver, arising in connection with veno-occlusive disease, chronic heart failure (CHF), Budd-Chiari syndrome, and profuse bleeding. Liver failure can develop with massive infiltration of the liver with tumor cells of lymphoma, metastasis of lung cancer, and pancreatic cancer.
Rare causes of liver failure include acute fatty liver dystrophy, autoimmune hepatitis, erythropoietic protoporphyria, galactosemia, tyrosinemia, and others. In some cases, the development of liver failure is associated with surgical interventions (portocaval shunt, transjugular intrahepatic portosystemic shunt, liver resection) or blunt trauma to the liver.
Factors provoking the breakdown of compensatory mechanisms and the development of liver failure may be electrolyte balance disorders (hypokalemia), vomiting, diarrhea, intercurrent infections, alcohol abuse, gastrointestinal bleeding, laparocentesis, excessive consumption of protein food, etc.
Symptoms of liver failure
The clinical picture of liver failure includes the syndromes of hepatic cell failure, hepatic encephalopathy, and hepatic coma. In the stage of hepatic cellular failure appears and progresses, jaundice, telangiectasia, edema, ascites, hemorrhagic diathesis, dyspepsia, abdominal pain, fever, and weight loss. With chronic liver failure, develop endocrine disorders accompanied by decreased libido, infertility, testicular atrophy, gynecomastia, alopecia, and atrophy of the uterus and mammary glands. Violation of metabolic processes in the liver is characterized by the appearance of the hepatic odor of the breath. Laboratory tests at this stage of liver failure reveal increasing levels of bilirubin, ammonia, and phenols in serum and hypocholesterolemia.
In the stage of hepatic encephalopathy, there are mental disorders: unstable emotional state, anxiety, apathy, sleep disorders, orientation, possible agitation, and aggression. Neuromuscular disorders are manifested by slurred speech, writing disorders, tremor of fingers, impaired coordination of movements (ataxia), increased reflexes.
The terminal stage of liver failure is hepatic coma. In the precoma phase, there is drowsiness, lethargy, confusion, short-term agitation, muscle twitching, convulsions, tremor, rigidity of skeletal muscles, pathological reflexes, uncontrolled urination. There may be bleeding gums, nosebleeds, or hemorrhages from the digestive tract. Liver coma occurs with a lack of consciousness and reaction to painful stimuli, fading reflexes. The patient’s face acquires a mask-like expression, pupils dilate and do not respond to light, BP decreases, and there is abnormal breathing. As a rule, at this stage of liver failure, the death of patients occurs.
Diagnosis of liver failure
When collecting anamnesis in patients with suspected liver failure, the facts of alcohol abuse, viral hepatitis, metabolic diseases, chronic liver disease, malignant tumors, and taking medications.
The study of clinical blood tests reveals anemia and leukocytosis. According to the coagulogram, signs of coagulopathy are determined: decreased PTI and thrombocytopenia. In patients with liver failure, a dynamic study of biochemical tests is necessary: transaminases, alkaline phosphatase, gamma-glutamyltransferase, bilirubin, albumin, sodium, potassium, and creatinine.
In the diagnosis of liver failure, the ultrasound data of the abdominal cavity are taken into account: with the help of echography, assess the size of the liver, the state of the parenchyma and vessels of the portal system, and exclude tumor processes in the abdominal cavity. Hepatic scintigraphy diagnoses diffuse liver lesions (hepatitis, cirrhosis, fatty hepatosis) and liver tumors and assess the rate of biliary secretion. If necessary, the examination of liver failure is supplemented with an MRI and CT of the abdominal cavity.
Electroencephalography is the main way to detect hepatic encephalopathy and the prognosis of liver failure. In the development of hepatic coma on EEG, slowing down and reduction in the amplitude of rhythmic activity waves are registered. Morphologic data of liver biopsy differ depending on the disease that led to liver failure. Liver encephalopathy is differentiated with subdural hematoma, stroke, brain abscess, tumors, encephalitis, and meningitis.
Treatment of liver failure
In liver failure, a diet with strict restriction or exclusion of protein is prescribed; in the precoma stage, probe or parenteral nutrition is provided.
Treatment of liver failure includes measures to detoxify, improve microcirculation, normalize electrolyte disorders, and acid-base balance. For this purpose, large volumes of 5% glucose solution, cocarboxylase, vitamins B6, B12, essence, and lipoic acid are administered intravenously.
To reduce the absorption of toxic substances, intestinal cleansing with laxatives and enemas is carried out. Short courses of broad-spectrum antibiotics and lactulose are prescribed, inhibiting the processes of putrefaction in the intestine.
Prednisolone is indicated for the development of hepatic cell coma; to combat hypoxia, oxygen inhalation or hyperbaric oxygenation is advisable.
In severe cases of liver failure, liver transplantation is recommended.
All these treatment options are available in more than 150 hospitals worldwide (https://doctor.global/results/diseases/hepatic-failure). For example, liver transplantation can be performed in these countries:
United States in 9 clinics
Germany in 14 clinics
Israel in 2 clinics
Turkey in 10 clinics.
Prognosis and prevention of liver failure
With timely intensive treatment of liver failure, liver dysfunction is reversible, and the prognosis is favorable. Liver encephalopathy in 80-90% passes into the terminal stage of liver failure – hepatic coma. A deep coma is the most often fatal outcome.
To prevent hepatic insufficiency, it is necessary for timely therapy of liver diseases, exclusion of hepatotoxic effects, drugoverdoses, and alcohol poisoning.