Definition and causes of the disease
Anterior cruciate ligament injury is one of the most severe knee injuries. It is accompanied by a clicking sensation in the knee and an inability to continue physical activity. The injury is followed by swelling and difficulty bending and extending the leg in the joint.
Prevalence
An anterior cruciate ligament (ACL) tear is a common knee injury. It occurs in 4 cases per 1000 people and is second only to meniscus injury. The ACL is the most traumatized ligament of the knee joint. In comparison, posterior cruciate ligament injuries are 15-30 times less common, as they are about 1.3-2 times thicker and two times stronger than the ACL.
In sports, ACL tears occur on average 4-10 times more often in women than in men. Presumably, this is due to weaker hamstrings. Hormonal factors may also influence the strength and flexibility of the ligaments.
Causes of ACL tears
Direct trauma – occurs when the thigh, shin, and knee are struck. It is more common in athletes, such as soccer players, wrestlers, and boxers. Less commonly, ligament tears occur in road traffic accidents.
Indirect injury – occurs when there is no direct blow to the knee joint. It can occur due to a sudden inward or outward deviation of the hip and torso. The tibia is rotated or fixed. Due to this deviation, a “twist” occurs in the knee joint, causing a ligament tear.
The ACL tears most often when the tibia is tilted outward and the femur is twisted inward. This injury is widespread among athletes, including soccer, handball, basketball, and volleyball players.
Often, in such an injury, in addition to tearing the ACL, the inner meniscus is damaged, and the inner collateral ligament is torn in severe twisting. This combination of injuries is called the “unlucky triad” or “knee explosion.” When the tibia is tilted inward, and the hip is twisted outward, a tear of the outer meniscus may join the ACL injury.
Symptoms of an anterior cruciate ligament tear
Symptoms of the acute period:
- a snap in the knee at the time of the injury;
- Inability to lean on the leg and continue physical activity;
- marked swelling of the knee joint, usually occurring within an hour of injury;
- symptoms of “pseudoblockage” – the patient cannot bend and straighten the leg in the joint.
Pathogenesis of anterior cruciate ligament rupture
The anterior cruciate ligament comprises spirally arranged collagen fibers that provide strength and stretchability. The ACL attaches at its upper end to the femur and at its lower end to the tibia. The ACL intersects with the posterior cruciate ligament in the middle of its course. These ligaments are named for their characteristic crossing.
The anterior cruciate ligament consists of three bundles:
- The anterior-internal ligament is the longest, most superficial, and most susceptible to injury. It is usually the one that is torn in partial ligament injuries.
- Posterior lies more profound than the previous one and is least prone to tearing.
- Intermediate.
The primary function of the ACL is to keep the tibia from shifting. Ligament tears are often caused by torsion on the supporting leg when the thigh and trunk rotate while the tibia and foot remain fixed. ACL damage leads to knee joint instability, i.e., discomfort from shifting the tibia relative to the hip.
If this condition lasts for a long time, the articular cartilage, menisci, and other joint structures wear out, and deforming osteoarthritis develops. This process proceeds at different rates, depending on both the traumatic agent and genetic predisposition. Over time, the patient begins to feel aching pain in the knee, first with prolonged loading and then at rest. The discomfort does not go away even when sleeping.
Classification and stages of an anterior cruciate ligament rupture
Types of ACL injury depending on the age and extent of injury:
- Acute lacerations;
- Long-standing tears and chronic instability;
- Partial tears and scarring of fibers;
- Rupture of the ACL together with the bone fragment.
Degrees of ACL injury:
- Minor ligament sprain (micro-tear). It is manifested by moderate swelling and pain. Movement is limited, butjoint stability is maintained.
- This is a moderate sprain (partial tear). Swelling and pain are more severe. Joint stability is preserved, but ligament strength is reduced, which can lead to multiple re-injuries.
- Complete rupture. It is manifested by severe swelling, intense pain, and instability in the joint. It is difficult tolean on the painful leg.
Complications of an anterior cruciate ligament tear
- knee contracture – decreased mobility of the knee in both flexion and extension;
- post-traumatic knee osteoarthritis;
- chronic instability of the knee joint.
Diagnosis of an anterior cruciate ligament rupture
Based on the symptoms described above, anamnesis data, special test results, and instrumental examination methods, it is possible to suspect a rupture of the ACL. Even in the acute period of injury, it is possible to assume the damage and make a final diagnosis. With a significant accumulation of blood in the joint cavity (hemarthrosis), the patient feels pressure in the knee joint; touching it is sharply painful, and there is a pronounced swelling.
Specific tests
When diagnosing ACL injuries, specific tests are mandatory.
- Lachman test: The leg is bent at the knee at an angle of 20-30 °, and the foot is lying on the couch. With one hand, the doctor fixes the thigh, encircling it in the distal part, and with the other hand, gently pulls the lower leg forward.
- Front drawer test – unlike the Lachman test, the leg is bent at a 90° angle.
Both methods can detect excessive tibial anterior displacement and determine its degree. The tests must also be performed on the healthy leg to compare the results.
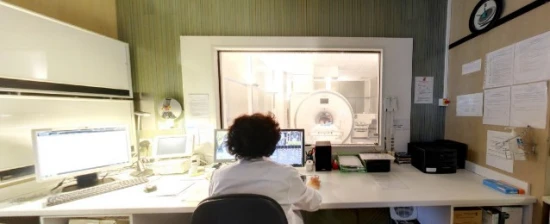
Instrumental diagnostic methods
The most informative method of diagnosing ACL injury is magnetic resonance imaging (MRI) of the knee joint. MRI allows for the visualization of soft tissues in the joint area and making a definitive diagnosis.
Signs of an ACL rupture:
- the ligament is not visualized;
- the continuity of her fibers has been compromised;
- an atypical arrangement of fibers;
- There are indirect signs: the ligament has a wavy contour, the tibia is displaced forward, and the posterior cruciate ligament is significantly deviated backward.
In the acute period, radiography is mandatory. The method allows to exclude or identify concomitant damage to bony structures, which may indicate a PCA rupture:
- Segond’s fracture is a detachment fracture of the tibial intercondylar eminence (anterior cruciate ligament attachment site). The ligament’s integrity is intact, but the characteristic symptoms of a tear are present.
- A ligament tear along with a bone fragment.
- Fracture of the head of the fibula.
Laboratory tests are not used to diagnose an ACL rupture because they do not provide any information about the condition of the joint.
Treatment of an anterior cruciate ligament tear
Pain, swelling, and inflammation should be eliminated in the acute period. In case of severe swelling of the knee joint, a puncture is performed to evacuate blood. Anti-inflammatory drugs are also prescribed. A cold is applied to the affected leg, and rest is ensured.
After the acute phase subsides, a fixator is indicated—a bandage, orthosis, or caliper. It is worn to stabilize the knee joint and start better rehabilitation. The main disadvantage is the strict selection of size and model.
Arthroscopic reconstruction is the only method that can fully restore joint function.
Grafts are used for surgery:
- Autografts – from the patellar ligament, the hamstring muscles tendons, and the peroneal muscle group.
- Allografts – from cadaveric material. There is a hypothetical risk of contracting infectious diseases (HIV, hepatitis, etc.), but it is negligible. However, not all countries have enough tissue banks, so such transplants are rarely used.
All manipulations on the joint are performed minimally invasively, i.e., through a few punctures and under the control of video equipment. It significantly reduces trauma and allows the patient to recover more quickly.
After surgery, the patient is observed in the hospital for 3-4 days. Anti-inflammatory and analgesic drugs are prescribed. Healing of postoperative wounds is also monitored; dressings on the wound are
regularly changed. A cast or rigid orthosis is applied to the operated leg for an average of two weeks. It creates immobility in the joint and reduces postoperative swelling and pain. During this period, you should walk with crutches, gradually increasing the load on the leg: in the first days after surgery without load, then every week increase by 25%, and by the 4th week, the full load is reached.
When normal gait is restored, crutches can be completely abandoned and the patient can roll from heel to toe. To accelerate healing and improve tissue nutrition in the joint area, you should perform a set of isometric exercises, i.e., contract the muscles without load.
Rehabilitation
After discharge from the hospital, the patient should see a rehabilitation specialist, who will explain how to proceed in detail. A set of physiotherapy treatments is prescribed to restore the function of the operated leg. A physiotherapist selects the methods strictly individually.
The patient will also need regular dressings at least once every 3-4 days. The stitches are removed on the 14th day after surgery. All these manipulations are carried out in the outpatient clinic.
Prognosis and prevention
With timely, adequate treatment and proper rehabilitation, the prognosis is favorable. In more than 95% of patients, joint function is fully restored.
On average, the artificially created ligament is fully engrafted by the fourth month after surgery. Subsequently, the graft is rebuilt, and its properties are as close as possible to those of the full-fledged “native” anterior cruciate ligament.
Without surgical treatment, the prognosis is unfavorable. Over time, deforming gonarthrosis will almost inevitably form. This complication requires unicondylar or total knee arthroplasty, a significant and traumatic operation to replace the knee joint with an artificial implant. Unfortunately, a system of clear and consistent measures does not exist to prevent ACL injuries. Proper warm-up, strengthening training, and special exercises in unstable conditions can help reduce the risk of injury for athletes. When running, jumping, and jerking, it is important to observe the correct technique. It is also important to follow the well-known safety rules in everyday life and at work.