Benign liver tumor treatment in 1 Oncology clinic in Norway
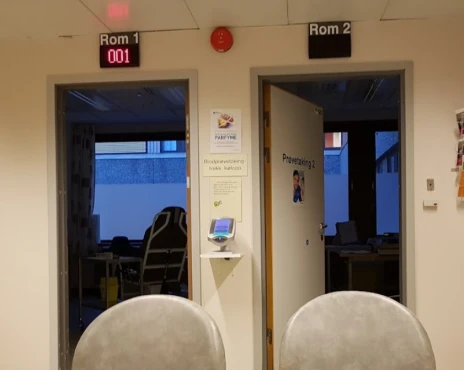
1 clinic specializing in Oncology providing treatment of
Benign liver tumor
A benign liver tumor refers to a non-cancerous growth in the liver. It can be asymptomatic or cause symptoms such as abdominal pain or discomfort. Treatment options depend on the type and size of the tumor and may include observation or removal.
Read more...
disease in Norway.
Besides this clinic there are 4 Oncology clinics in Norway.
Such diseases are treated by Aleris Frogner: Benign liver tumor, Bile duct cancer, Hepatolithiasis, Liver cancer, Liver cyst, and others.
Sorted by:
Relevance
Rating
Relevance
4 nearby similar clinics in Norway
Perhaps you should consider 4 more clinics we have found nearby basing on your Location, Disease filters applied.
Prices for popular procedures:
Prices for popular procedures:
Prices for popular procedures:
Countries with the highest number of clinics treating the diseases:
Benign liver tumor:
worldwide
631 clinics
Brazil
39 clinics
Germany
39 clinics
India
38 clinics
Colombia
25 clinics
Russia
25 clinics
Related procedures:
Procedures are likely to be used for Benign liver tumor treatment:
Chemoembolization,
Major liver resection,
Microwave tumor ablation (MWA),
Minor liver resection,
and
Non-anatomic liver resection (NAR)
.