Disease Types & Epidemiology
How common is the skin cancer?
Skin cancer stands out as the prevailing type of cancer in both the United States and across the globe. According to the American Academy of Dermatology, it is estimated that approximately 9,500 people in the US are diagnosed with skin cancer every day.
It encompasses three main types: basal cell carcinoma, squamous cell carcinoma, and melanoma. BCC and SCC, also known as non-melanoma skin cancers, account for the majority of cases, with over 5 million diagnoses registered annually in the United States.
Conversely, although less frequent, melanoma poses a more significant threat given its propensity to metastasize to other body parts. More than 1 million Americans are living with melanoma. The American Cancer Society estimates that about 100,640 new cases of melanoma will be diagnosed in the United States in 2025, resulting in approximately 8,290 deaths.
Types of Skin Cancer
- Basal Cell Carcinoma (BCC) - makes up approximately 80% of all skin cancers. It starts in the basal cells located at the bottom layer of the epidermis. BCCs typically have slow growth and seldom metastasize, but if left untreated, they can cause considerable damage to the local area. They manifest as shiny bumps or flat patches with a flesh-like color.
- Squamous Cell Carcinoma (SCC) - accounts for approximately 20% of skin cancers, and it originates in the squamous cells found in the middle and outer layers of the skin. Unlike basal cell carcinomas, SCCs have a greater propensity to form large masses and a higher tendency to spread into body areas other than skin. They commonly manifest as red, scaly patches or nodules.
- Melanoma - is the most fatal type of skin cancer, emerging from the melanocytes which produce skin pigment. Despite being only 1% of all skin cancer cases, it leads to the majority of skin cancer fatalities. Melanomas can appear on any body part and frequently look like moles or develop from existing ones. Timely identification is crucial as melanoma has the potential to spread rapidly.
Causes & Risk Factors
What is the primary issue of skin cancer?
Excessive exposure to ultraviolet radiation from the sun or tanning beds is the leading factor behind skin cancer. While UV radiation can harm the DNA in skin cells, causing mutations that have the potential to lead to cancer, various factors also elevate the likelihood of developing this condition:
- Skin Type. People with pale skin, light-colored hair, and light eyes have a higher risk of developing skin cancer because they have lower levels of melanin, which provides a natural defense against UV radiation.
- Family History. A family background with a history of skin cancer raises an individual's susceptibility. For instance, having a close relative who has had melanoma elevates the risk by two to three times.
- Moles. Having numerous or unusual (dysplastic) moles raises the chances of developing melanoma.
- Immune Suppression. Individuals who have compromised immune systems, such as those who have undergone organ transplants, face a greater susceptibility to skin cancer.
- Exposure to Toxic Substances. Exposure to certain chemicals, such as arsenic, can increase the risk of developing skin cancer.
Clinical Manifestation & Symptoms
What signs should one anticipate while suspecting skin cancer?
Skin cancer can manifest in different ways, depending on its type. There are the following key symptoms to be mindful of:
- Basal Cell Carcinoma (BCC):
- Pearly or wax-like lumps, flat, skin-colored, or brown marks, or persistent sores that bleed and fail to heal.
- Squamous Cell Carcinoma (SCC):
- Red, rough patches or raised areas with a recessed center that might form crusts or bleed.
- Melanoma:
- The changes in current moles or the development of new, abnormal growths that follow the ABCDE guideline - a valuable tool for detecting possible melanomas:
- Asymmetry: One half of the mole does not match the other half.
- Border: Edges are irregular, ragged, notched, or blurred.
- Color: Color is not uniform and may include shades of brown or black, sometimes with patches of pink, red, white, or blue.
- Diameter: The spot is more significant than 6 millimeters across (about the size of a pencil eraser).
- Evolving: The mole is changing in size, shape, or color.
- The changes in current moles or the development of new, abnormal growths that follow the ABCDE guideline - a valuable tool for detecting possible melanomas:
Diagnostic Route & Screening
When, where, and how should skin cancer be detected?
The timely identification of skin cancer is essential for successful treatment. The diagnostic procedure usually includes:
- Self-Examination:
- Regular self-examinations can help identify suspicious changes in the skin early. It is recommended that self-exams be performed monthly, using mirrors to check hard-to-see areas.
- Clinical Examination:
- A thorough examination of the skin is always part of routine check-ups with a dermatologist, and they will also carefully assess any suspicious lesions.
- Biopsy:
- If an unusual area is discovered, a biopsy is conducted to extract a tissue sample for microscopic analysis. This procedure validates the diagnosis and identifies the specific type of skin cancer.
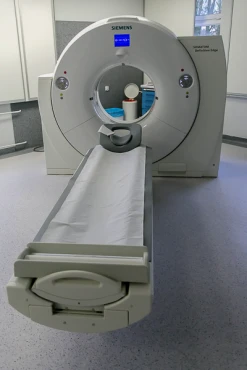
- Imaging Tests:
- CT scans, MRIs, or PET scans are employed to evaluate the spread of suspected cancer. Cancer Research UK.
Treatment Approaches
What are the options for managing skin cancer?
- Surgery:
- Excisional surgery: The most common treatment for BCC and SCC involves removing the tumor and a portion of healthy tissue surrounding it.
- Mohs surgery: An exact surgical method that involves the gradual removal and examination of thin layers of skin containing cancer cells until only healthy tissue remains. This approach is especially valuable for treating significant, recurrent, or challenging-to-treat skin cancers.
- Curettage and Electrodesiccation: The tumor is removed, and the area is then treated with an electric needle to eliminate any remaining cancer cells.
- Radiation Therapy:
- External Beam Radiation: High-dose radiation is employed to pinpoint and eliminate cancerous cells. This approach is frequently utilized for cancers that present challenges for surgical treatment or for individuals who are not candidates for surgery.
- Cryotherapy:
- Cryosurgery: Liquid nitrogen is commonly used to freeze and eradicate irregular cells, often for precancerous conditions and treating small, early-stage skin cancers.
- Topical Treatments:
- Topical Chemotherapy: 5-fluorouracil (5-FU) treats precancerous lesions and superficial skin cancers directly on the skin.
- Imiquimod is a cream that activates the body's immune system to target and destroy cancer cells. It is prescribed for treating superficial BCC and actinic keratosis, a precancerous skin condition.
- Targeted Therapy:
- Vismodegib and Sonidegib: These medications block the Hedgehog signaling pathway, which is typically active in most BCCs. They are prescribed for advanced or metastatic BCC that is not amenable to treatment through surgical or radiation methods.
- Immunotherapy:
- Pembrolizumab and Nivolumab help the body's immune system fight melanoma cells, leading to better survival rates for advanced melanoma.
Prognosis & Follow-up
How does cutting-edge science improve the lifespan and quality of life for those with the disease?
The prognosis for skin cancer varies depending on the type and stage at diagnosis.
- Basal cell carcinoma demonstrates a high likelihood of recovery, boasting a success rate of over 95% when identified and addressed in its early stages.
- When treated promptly, SCC also boasts a high remission rate, with roughly 95% of patients surviving for at least five years after diagnosis.
- The outlook for melanoma depends a lot on when it's found. The 5-year survival rate is about 99% if the cancer is caught early but drops to around 65% if it has spread nearby and goes down to 25% if it has reached distant organs.
Regular skin checks are crucial for detecting new or returning skin cancers early on. The frequency of these examinations is determined based on the patient's risk factors and the type of cancer being treated. Typically, follow-up appointments are scheduled every 3 to 6 months in the initial years post-treatment, shifting to annual check-ups afterward. Patients with a history of multiple skin cancers or those at elevated risk may require more frequent monitoring.
Patients should make it a habit to conduct frequent self-assessments to identify any new or evolving lesions. This entails carefully examining all areas of the skin, even those that are not easily visible, and using mirrors when necessary. Any changes observed should be promptly communicated to a healthcare provider.
Patients should be informed about the vital role of sun protection in preventing skin damage and reducing the risk of new skin cancers. This involves using broad-spectrum sunscreen with an SPF of 30 or higher, wearing protective clothing, and avoiding tanning beds and excessive sun exposure.