Introduction
Melanoma is one of the most severe types of skin cancer because it spreads beyond the skin more often than most other skin cancers. However, if discovered early, it is curable with the proper treatment.
Melanoma occurs when something goes wrong in melanocytes (the pigment cells that produce melanin). When skin cells are damaged, new cells may grow out of control and form a mass of cancerous cells.
Melanoma often occurs in people over 50 years of age. It can also occur in people of younger age and even in children.
The most evident link is exposure to UV radiation from the sun or tanning devices. Exposure to UV radiation causes changes to the DNA (genetic material) of pigment cells and increases the risk of melanoma. However, melanoma can be found in areas with little or no sun exposure, such as the soles of feet, palms of hands, and underneath fingernails (called acral lentiginous melanomas). People with darker skin are more likely to develop melanoma in areas less exposed to the sun.
Melanoma can also occur in the nail bed, on internal mucosal surfaces such as in the mouth, on the tongue, or in the intestines (mucosal melanoma), in the genital areas, and in the eyes (ocular melanoma).
A specific type of melanoma – so-called hereditary melanoma - is linked to a family history of malignancies, such as skin (cutaneous) melanoma, eye (uveal) melanoma, pancreatic, kidney, or breast cancer, astrocytoma (cancer of the brain or spinal cord), mesothelioma (cancer of the tissue that covers internal organs).
Diagnosis and staging
What evaluations do melanoma patients undergo to identify the best treatment strategy?
Because melanoma has an irregular shape and different colors, using the standardized ABCDE rule to detect this type of skin cancer is crucial.
Asymmetry – One half of a mole or spot does not match the other half.
Border – The edges of a spot seem irregular and are challenging to define.
Color – The spot's color is not the same throughout (it may be brown, black, or sometimes with patches of pink, red, white, or blue).
Diameter – The spot is larger than 6 millimeters across (about the size of a pencil eraser).
Evolving – The spot or mole changes its size, shape, or color.
There are several abnormal (mutated) genes related to hereditary melanoma. They include:
- A CDKN2A mutation, which is the most common gene mutation. It is also called p16INK4A or MTS1. It often means that many cases of melanoma that were found at an early age run in the patient's family.
- The melanocortin-1 receptor (MC1R) gene helps determine a patient's skin color. MC1R can determine if the patient or the patient's family members have red hair and/ or fair skin, which increases the patient's risk of developing melanoma.
- BAP1 gene mutations, which can cause uveal and cutaneous melanoma.
Thus, genetic testing is one of the procedures during diagnostic work-up.
Melanoma staging
The American Joint Committee on Cancer (AJCC) TNM staging system is widely used to stage melanoma. In this system, the letters T, N, and M describe different areas of cancer growth. The physician will assign a score or number to each letter based on cancer test results. The higher the number, the larger the tumor or the more the cancer has spread. An example of this is T1, N0, or M0.
Tumor depth (T) – refers to the thickness of the primary tumor and whether the tumor has broken through the skin (this is called ulceration). This is measured in millimeters (mm).
Lymph node status (N) – refers to whether the cancer has spread nearby through small tubes called lymph vessels or to small bean-shaped structures called lymph nodes.
Metastasis (M) – describes whether the cancer has spread to parts of the body far away from the primary tumor and distant lymph nodes.
The TNM stages will be combined to assign the cancer stage group. There are five stages of melanoma. Often, physicians write stages 1 through 4 as Roman numerals—stages I, II, III, and IV.
Stage 0 to 2
Stage 0, stage 1, and stage 2 melanoma are cancers in the skin that are not known to have spread elsewhere.
Stage 0 melanoma in situ refers to melanoma found only in the outermost layer of skin (epidermis). This early stage very likely has not yet spread to other body parts and is cured when completely removed.
Stage 1 melanoma enters the skin's second layer, called the dermis. When melanoma reaches the dermis, it is described as invasive. Stage 1 is a lesion (tumor) thinner than or equal to 2 mm (Breslow depth). Stage 1 melanoma may or may not show ulceration, though most do not.
Stage 2 refers to tumors that are 1 to 2 mm thick and have ulceration or tumors that are thicker than 2 mm with or without ulceration. A person with stage 2 melanoma has a higher chance of cancer spreading beyond the primary tumor than a person with stage 1 melanoma.
Stage 3
Stage 3 melanoma is known as regional melanoma. It is considered an advanced form of cancer. In this stage, the melanoma has spread to nearby lymph nodes or lymphatic vessels in the skin, called in-transit or satellite metastasis.
Stage 4
Stage 4 melanoma is determined when the cancer has spread from the primary tumor to distant body areas such as the lungs, liver, brain, bones, or gastrointestinal (GI) tract.
Algorithm of diagnosis
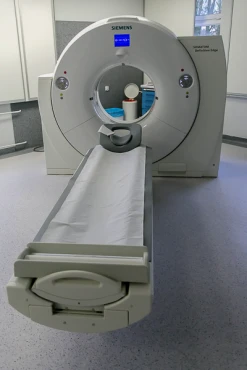
Besides clinical examination and imaging (CT/MRI/PET scans), one critical diagnostic approach ultimately defines the diagnosis – the biopsy. This procedure includes taking the tumor tissue to the lab for biomarker testing. The typical cellular markers for melanoma are BRAF gene mutations, with the most common form BRAF V600E.
Skin biopsies are done using a local anesthetic (numbing medicine) injected into the area with a tiny needle. A skin lesion biopsy can be incisional (does not altogether remove the lesion) or excisional (completely removes the lesion).
An excisional or complete biopsy is preferred for finding melanoma because it removes a larger skin area than an incisional or partial biopsy. It can be done through an elliptical (total thickness) removal method, a punch method, or a deep shave removal method (also called a saucerization biopsy).
- Elliptical biopsy
An elliptical excisional biopsy removes an area of skin, usually in a fusiform (an oval "football") shape. A rim of normal-looking tissue surrounding the lesion will be removed, too. This normal-looking tissue is called the margin. Elliptical biopsy uses stitches to close the wound.
- Punch biopsy
For a punch biopsy, a small piece of skin and connective tissue are removed using a hand-held tool. Tiny stitches are then used to close the opening in the skin. One or more punch biopsies may be used on extensive lesions where a complete/excisional biopsy isn't possible. This can help to avoid inaccurate pathology results.
- Deep shave (saucerization) biopsy
A shave biopsy can be done either on the skin surface (superficial) or deeper. Superficial shave biopsies (also called broad or shallow biopsies) can be used when a lesion is likely not cancerous. They are generally not recommended when melanoma is suspected. Superficial shave biopsies may be helpful for certain melanoma types that show flat skin lesions.
Deep shave biopsies are used for most melanoma diagnoses to remove the suspicious skin lesion completely. This biopsy is also called a scoop biopsy or saucerization/shave removal. This type of biopsy removes the top layer of skin (epidermis) and part of the underlying layer (dermis) using a tool similar to a razor.
- Lymph node biopsy
A lymph node might be biopsied if the physician suspects it has cancer cells. Lymph nodes are usually too small to be seen or felt.
Lymph nodes may be cancerous if they feel swollen, enlarged, stiff to the touch, or don't move when pushed (they are fixed or immobile). A lymph node biopsy can be done using a needle or as a minor surgery to remove a lymph node.
Treatment routes
What is an appropriate treatment for different melanoma stages?
Surgery is the primary (first) treatment for almost all melanomas. A person diagnosed with melanoma should expect some surgery to follow the skin biopsy. The goal of surgery is to remove all the cancer from the patient's body. Surgery may be the only treatment needed for melanomas with a low risk of spread.
- Wide excision removes the melanoma tumor as well as some normal-looking tissue surrounding it (the surgical margin). The surgical margin is measured in centimeters (cm). The size to be removed depends on the thickness of the primary tumor: for in situ melanoma – 0.5-1 cm margin around the tumor lesion; <1 mm lesion thickness – 1 cm margin; 1-2 mm – 1-2 cm margin; >2 mm tumor thickness – 2 cm margin.
Most stage 0 and stage 1 melanoma are treated under local anesthesia. For deeper or more advanced melanomas that require lymph node biopsy or surgery, general anesthesia may be used.
A wide excision is done even if the melanoma tumor was removed by biopsy. A wide excision will also remove lymphatic channels in the skin because there could be additional tumor cells and any nearby microsatellites. Lymphatic channels are thin-walled, tube-like vessels, like blood vessels, that carry a fluid called lymph.
A skin graft might be recommended after the surgery to cover the wound. Skin grafting involves removing skin from one body area and moving it to a different location.
- Sentinel lymph node biopsy is the first lymph node to which cancer cells most likely spread from a primary tumor. Sometimes, there is more than one sentinel lymph node. Many people with melanoma have an SLNB at the same time as the wide excision.
- A lymph node dissection may occur if the cancer has spread to the lymph node basin. A lymph node dissection removes the nodes to prevent the disease from returning or spreading elsewhere. This surgery is done under general anesthesia. Lymph node dissection is generally reserved for advanced melanomas with nearby enlarged lymph nodes. Newer therapy options are lessening the need for this type of surgery for stage 3 melanoma.
Targeted therapy drugs are designed to target cancer cells specifically. For melanoma, these drugs target the activity of a specific or unique feature of melanoma cancer cells and interfere with how those cancer cells grow.
Cancer growth inhibitors – block tumor growth factors. There are several subgroups based on the mechanism of action, such as
-
- BRAF inhibitors that attack the BRAF tumor-stimulating protein (vemurafenib, dabrafenib, and encorafenib).
- MEK inhibitors against MEK protein – trametinib, cobimetinib, and binimetinib.
- KIT inhibitors – for rare KIT mutations melanoma – imatinib, dasatinib, and nilotinib.
Immunotherapy - uses the immune system to kill cancer cells. The body's defense against disease is called the immune system. T-cells are a crucial part of this system. T-cells that kill infected and cancer cells are called cytotoxic or killer T-cells.
- Checkpoint inhibitors release significant stimulation of T-cells, such as pembrolizumab and nivolumab.
- T-VEC – talimogene laherparepvec - is a weakened form of the herpes virus made in a lab. T-VEC enters and destroys melanoma cells.
- Imiquimod – immune response modifier in a cream form that stops abnormal skin growth.
Chemotherapy (dacarbazine, temozolomide) and radiation therapy (external beam / intensity-modulated / image-guided radiotherapy) are used in advanced and recurrent cases of melanoma.