Disease types & Epidemiology
How common is the disease?
Varicose veins are a prevalent condition, particularly affecting the lower limbs. In this condition, the veins become enlarged, twisted, and often visible under the skin. This occurs when the valves in the veins, which regulate blood flow, weaken or become damaged, causing blood to accumulate. Varicose veins are more common in women and older adults, with an estimated 23% of U.S. adults experiencing this condition. It is particularly prevalent in individuals aged 40 and above, with women being twice as likely as men to develop varicose veins [Society for Vascular Surgery, American Venous Forum, 2024].
Causes & Risk factors
What is the primary issue of varicose veins?
Varicose veins are primarily caused by the weakening of the one-way valves within the veins that help maintain proper blood flow in the legs. When these valves malfunction, blood can flow backward and accumulate in the veins, causing them to become enlarged.
Several factors can increase the risk of developing varicose veins:
- Age: The risk rises as people get older because veins lose elasticity, and their valves become weaker.
- Gender: Women are more prone to varicose veins due to hormonal changes during pregnancy, menstruation, and menopause. Hormonal medications like birth control pills may further increase the risk.
- Pregnancy: The increased blood volume and pressure during pregnancy can enlarge veins, especially in the legs.
- Genetics: Having a family history of varicose veins increases one's chances of developing the condition.
- Obesity: Excess weight adds pressure on the veins, increasing the risk.
- Occupation: Jobs that require prolonged standing or sitting, such as nursing, teaching, and factory work, can increase the risk due to poor circulation.
Clinical manifestation & Symptoms
What signs should one anticipate while suspecting varicose veins?
Varicose veins manifest as visibly enlarged, twisted veins that are often blue or dark purple in color. People with this condition commonly experience various symptoms. For instance, they may feel pain or aching in their legs, especially after prolonged standing or sitting. Swelling in the lower legs, ankles, or feet is another common symptom. Individuals may also experience a heaviness or throbbing sensation in their legs. In severe cases, skin discoloration or ulceration around the ankles can occur. Some people even report itchiness or a burning sensation in the affected veins.
In some instances, varicose veins can lead to more serious complications, such as phlebitis (inflammation of the vein), deep vein thrombosis (formation of a blood clot), and venous ulcers. These complications indicate the need for more aggressive treatment to address the underlying venous issues and prevent further complications.
Diagnostic route
When, where, and how should the varicose veins be detected?
Diagnosing varicose veins typically begins with a physical examination by a healthcare provider. They will closely inspect the visible veins and inquire about symptoms such as leg pain, swelling, and general discomfort [University of Tennessee, 2023].
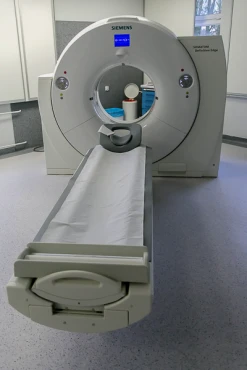
To confirm the severity of the varicose veins, healthcare providers have several diagnostic tools at their disposal. One common method is duplex ultrasound, a non-invasive procedure that uses sound waves to assess the structure and blood flow within the veins. This test can help detect any issues with venous reflux or the presence of blood clots.
Another, albeit less frequently used, technique is venography. This imaging procedure involves injecting a contrast dye into the veins, allowing the provider to visualize any abnormalities more clearly. Venography is often reserved for cases where complications like deep vein thrombosis are suspected.
Additionally, physicians may utilize photoplethysmography, a test that measures venous function by analyzing blood flow in the legs. This can be particularly useful for patients who may have venous insufficiency without visible varicose veins.
Treatment approaches
What are the options for managing varicose veins?
Managing varicose veins typically involves a combination of conservative and invasive treatments, depending on the severity of the condition and associated symptoms [Academy of Medical Royal Colleges, 2024].
Lifestyle modifications can help improve circulation and alleviate symptoms in mild cases. Regular exercise, such as walking, promotes blood flow, while compression stockings apply pressure to the legs, assisting veins and muscles in moving blood more efficiently. Elevating the legs when resting can also help reduce swelling.
For smaller varicose and spider veins, sclerotherapy is a non-surgical treatment that involves injecting a solution directly into the affected veins. This solution irritates the vein walls, causing them to collapse and be reabsorbed by the body. Sclerotherapy has a high success rate of 75-90% after several sessions.
Endovenous laser ablation is a minimally invasive technique that uses laser energy to close off larger veins. A catheter is inserted into the vein, and laser energy is applied to seal the vein shut, allowing the blood to reroute to healthier veins. EVLA boasts a 98% efficacy rate and is commonly used for more significant varicose veins.
Similarly, radiofrequency ablation uses radiofrequency energy to heat and close off problematic veins. RFA is known for faster recovery times and minimal post-procedural pain, with success rates of 94-97%.
In more severe cases, surgical options, such as vein stripping, where veins are tied off and removed, may be considered. However, these procedures are more invasive and come with a longer recovery time. With the advancements in less invasive methods, this approach is becoming less common.
Foam sclerotherapy is a variation of traditional sclerotherapy and can be used to treat larger veins. This method has a success rate of 80-85% and is often used in combination with other treatments.
Prognosis & Follow-up
How does cutting-edge science improve the lifespan and quality of life for those with varicose veins?
With appropriate treatment, most patients experience relief from their symptoms. Minimally invasive options like sclerotherapy and endovenous laser therapy have shown high success rates and low recurrence when combined with lifestyle changes. However, it's important to note that varicose veins can potentially reoccur, especially if the underlying venous insufficiency is not properly addressed. Studies indicate that up to 20-30% of patients may develop new varicose veins within five years of their initial treatment.
To ensure the best long-term outcomes, healthcare providers typically follow a standard protocol. This typically involves a check-up around 6 weeks after the initial treatment to assess immediate results and determine if any additional interventions are needed. Patients are then scheduled for follow-up appointments, usually between 6 months to 1 year post-treatment, to monitor for any recurrence and evaluate the overall health of their veins.
Patients are often advised to continue using compression stockings to improve circulation, particularly if they have a history of venous insufficiency. Maintaining a healthy lifestyle, which includes regular exercise and weight management, can also help prevent the reoccurrence of varicose veins.