Introduction
Adrenoleukodystrophy is an inherited pathology from the group of peroxisomal diseases associated with the accumulation of fatty acids with a very long carbon chain in the body. The disease is characterized by clinical polymorphism – different forms are characterized by damage to brain tissue and adrenal glands, manifested by a combination of neurological disorders (sensorimotor, emotional-cognitive, behavioral) and hypocorticism. Diagnosing the pathology according to clinical data and confirming with biochemical, molecular genetic tests, MRI, and CT brain. Complex treatment involves diet, pharmacotherapy, and transplantation of hematopoietic cells.
General information
Adrenoleukodystrophy (Zimmerling-Kreutzfeldt, Addison-Schilder disease) is not as rare as previously thought – it occurs everywhere, surpassing other peroxisomal diseases in prevalence. According to various studies, the frequency of this variant of leukodystrophy varies from 1:100000 to 1:15000; the pathology affects representatives of all age groups (children, adolescents, adults). Usually, males are affected, and females are carriers of the mutant gene, but in 20% of cases with heterozygous genotypes, symptoms are also found in them.
Causes of adrenoleukodystrophy
The pathology is associated with mutations in the ABCD1 gene, which occupies the terminal region of the long arm of the X chromosome (locus Xq28). It encodes the synthesis of a transmembrane transfer protein called adrenoleukodistophic protein (ALDP). The latter is located on specific cell organelles involved in oxidation reactions – peroxisomes, responsible for the transportation and further breakdown of very long-chain fatty acids.
Pathogenesis
Due to the structural abnormality of the transfer protein, the transport of fatty acids into peroxisomes, where they should undergo β-oxidation, is impaired. Usually, saturated long-chain fatty acids are present in lipids of nervous tissue (cerebroside, sulfatides) and erythrocytes, but in adrenoleukodystrophy, their content can increase a thousand times. Abnormal ones replace ordinary cholesterol esters with chain lengths of 24-30 or more carbon atoms. When their concentration in the nerve fiber sheath reaches 10%, myelin is destabilized and destroyed.
Accumulation of fatty acid derivatives disturbs the physicochemical properties of cell membranes: mitochondrial permeability increases, and cytosolic calcium concentration increases. In turn, this leads to the atrophy of adrenal neuroendocrine tissue. An essential mechanism of demyelination is the activation of neuroglial structures and stimulation of inflammatory processes with the participation of cytokines (tumor necrosis factor).
Histological changes in cerebral variants of adrenoleukodystrophy are characterized by a sharp decrease in myelin content and perivascular lymphocytic-macrophage infiltration. The demyelinating process begins with the corpus callosum and gradually moves to the white matter of the occipitoparietal regions. The involvement of frontal lobes and the pyramidal tract is observed less frequently.
Classification
A pronounced phenotypic polymorphism characterizes adrenoleukodystrophy due to differences in penetrance and expression of the abnormal gene. Taking into account the time of debut, the main manifestations, and the rate of symptom onset, modern neurology distinguishes several forms of the disease:
- Cerebral. Neurological disorders prevail among the symptoms. Based on the age at which the disease began, the child, juvenile, and adult forms are distinguished. The first occurs more often than the others (48%).
- Adrenomyeloneuropathy is the most common variant in adult patients (26% of cases). It is characterized by a combination of corticoid insufficiency and spinal disorders.
- Isolated adrenal insufficiency usually proceeds without affecting the nervous system. In the overall structure of adrenoleukodystrophy, isolated hypocorticism is assigned a tenth part.
- Asymptomatic, with no clinical manifestation, is manifested only by a biochemical defect in the cleavage of fatty acid molecules. It usually occurs in relatives of patients but can be considered a preclinical stage.
- Symptomatic in heterozygous carriers. The disease is accompanied by the simultaneous presence of the dominant and recessive allele of the mutant gene in the genotype in middle-aged women. It accounts for less than 1% of the cases.
- Atypical. It is characterized by cerebellar disorders – isolated or combined with adrenal insufficiency. It is extremely rare.
Symptoms of adrenoleukodystrophy
The clinical picture of the pathology is very variable, determined by the specific phenotypic variant. Clinicians most often have to deal with signs of cerebral form, adrenomyeloneuropathy, or isolated adrenal insufficiency.
Cerebral form
All varieties of cerebral adrenoleukodystrophy are characterized by rapid progression. The peak manifestation of the pediatric form occurs between 5 and 10 years of age. In most patients, neuropsychiatric disorders precede signs of adrenal insufficiency. Disorders of behavior, thinking, and motor sphere are characteristic. Children become hyperactive or autistic and episodically show aggression. There is an attention deficit, progressive dementia, and disturbed gait.
Hypocorticism is manifested by skin pigmentation, muscle weakness, periodic nausea, and vomiting. Progression of the pathological process is accompanied by spastic tetraparesis, blindness, and deafness; there are drug-resistant seizures. Death occurs within a year to 15 years from the onset of the disease.
Adrenomyeloneuropathy
The disease begins in a wide age range, from 12 to 50 (more often between the second and fourth decades of life). In many cases, symptoms of chronic hypocorticism precede or accompany neurologic disorders. Sometimes, the first sign, occurring long before the entire clinical picture unfolds (in early childhood), is isolated skin hyperpigmentation.
Initial neurological signs are represented by myelopathy with decreased deep sensitivity and lower paraparesis. Further development of such adrenoleukodystrophy is manifested by tetraparesis with impaired function of pelvic organs (urination, defecation, erection).
Isolated adrenal insufficiency
The lesions of the adrenal cortex are manifested first by glucocorticoid and then by mineralocorticoid deficiency, debuting at various times starting at the age of two. The most frequent symptoms are loss of appetite, muscle weakness, and vomiting. Patients lose weight, suffer from abdominal pain, and have hypotension.
Symptomatic adrenoleukodystrophy
In some female carriers, the onset of neurologic symptoms without accompanying endocrine shifts is noted. The disease debuts later than in men with spinal lesions – by the age of 50-60 years. In severe cases, the symptomatology is similar to the cerebral form, while moderate disorders resemble adrenomyeloneuropathy.
Complications
Progression of cerebral forms and adrenomyeloneuropathy is accompanied by severe neurological deficits with disability. A dangerous complication of hypocorticism is acute decompensation with the development of a crisis manifested by dehydration and cardiovascular and renal failure. Rapidly progressive variants without active correction end in coma and death.
Diagnosis
It is possible to assume the disease with careful evaluation of anamnestic information (presence of family cases, the time of manifestation, the nature of the course) and clinical data. However, the pathogenetic features of adrenoleukodystrophy are established with a comprehensive laboratory and instrumental study. The diagnostic program includes the following methods:
- Biochemical blood tests. Mass spectrometry detects fatty acids in plasma or cells (erythrocytes, leukocytes, skin fibroblasts) and is considered a method of early diagnosis (screening). The other biochemical indicators necessarily examine cortisol levels, ACTH, and electrolytes.
- Molecular genetic tests. Direct sequencing is used to detect gene mutations. The pathology is characterized by a high frequency of unique mutations. The correlation between the results of molecular genetic studies and the severity of the disease cannot be established.
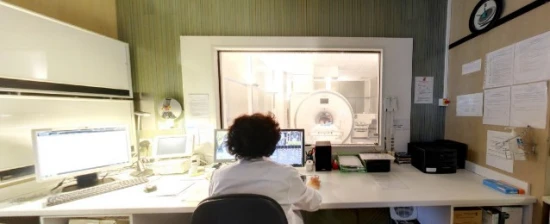
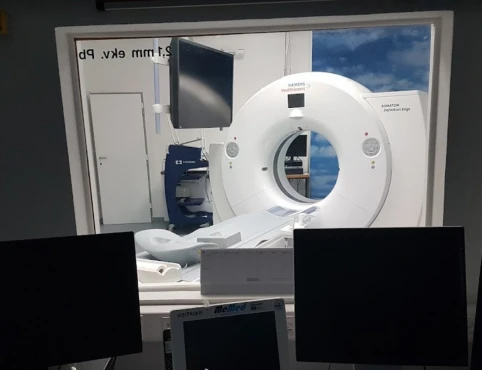
- CNS tomography. In individuals with cerebral forms, MRI reveals a symmetric decrease in signal intensity in areas of the corpus callosum and corticospinal tract with transition to the occipital-parietal zone. Progression of adrenoleukodystrophy is accompanied by accumulation of contrast agents in the foci of demyelination. CT scan reveals weakening of the intensity of the white cerebral substance and calcifications.
- EMG. Patients with adrenomyeloneuropathy may undergo electroneuromyography, which shows a decrease in motor and sensory response amplitude. When analyzing stem-evoked potentials (visual, auditory, somatosensory), a slowdown of impulse conduction velocity is recorded.
Treatment of adrenoleukodystrophy
Conservative therapy
Choosing reasonable pathogenetic therapy is clinicians’ most acute problem when treating a particular patient. Since the disease can be diagnosed even before the development of clinical signs, presymptomatic correction is of particular importance. Conservative methods are used in the treatment of adrenoleukodystrophy:
- Diet. A low-fat diet is recommended to normalize the level of fatty acids in the blood. Diet is effective only at the preclinical stage of the disease.
- Pharmacotherapy. In the phenomenon of hypocorticism, replacement therapy with glucocorticoids and mineralocorticoids is clearly indicated, but these drugs have no effect on the pathological process in the central nervous system. Neurometabolic agents, myorelaxants, and vitamins are used to treat myelopathy symptomatically.
- Bone marrow transplantation. In the early stages of adrenoleukodystrophy in childhood and adolescence, allogeneic transplantation of hematopoietic stem cells can stop the progression of demyelination, so it is recognized as the primary treatment method.
Prognosis and prevention
The long-term prognosis in X-linked adrenoleukodystrophy depends on the specific phenotype. In children, the cerebral form has a particularly severe, rapidly progressive course with a five-year survival rate of 59%, with many dying within a few years of disease onset. Other forms may not affect life expectancy but may reduce the quality of life through disability. Given the high degree of polymorphism, even among members of the same family, prognosis can vary considerably.
Primary prevention measures in adrenoleukodystrophy involve medical and genetic counseling of probable carriers and prenatal diagnosis (biopsy of chorionic villi, analysis of amniotic fluid). Early detection of biochemical changes in the blood is essential to confirm the diagnosis at preclinical stages. In combination with active pathogenetic therapy, it will help to avoid progression, reducing the risk of further disability.