Definition
Perthes disease is a partial aseptic necrosis of the head of the femur. The disease occurs in adolescence or childhood. The onset is gradual. There are minor pains in the joint, a slight limp or "plantar flexion" of the leg is also possible. Later, the pain becomes intense, there is a pronounced limp, swelling, and weakness of the muscles of the limb, and contractures are formed. In the absence of treatment, the likely outcome is deformation of the head and the development of coxarthrosis. Diagnosis is made based on symptoms and radiologic picture. Long-term, conservative treatment includes immobilization, therapeutic exercises, massage, and physiotherapy. In severe cases, reconstructive and restorative surgeries are performed.
General information
Perthes disease is a pathological process characterized by impaired blood supply and subsequent femoral head necrosis. It is a fairly common disease and accounts for about 17% of the total number of osteochondropathies. Children from 3 to 14 years of age suffer from it. Boys suffer 5-6 times more often than girls, but girls tend to have a more severe course. Both unilateral and bilateral lesions are possible, with the second joint usually suffering less and recovering better.
Causes
Currently, no single cause of Perthes disease has been identified. It is believed that it is a polyetiologic disease, in the development of which a certain role is played by both the initial predisposition and metabolic disorders, as well as environmental influences. According to the most common theory, Perthes disease is observed in children with myelodysplasia - congenital underdevelopment of the lumbar spinal cord, a common pathology that may not manifest itself in any way or become the cause of various orthopedic disorders. It is assumed that the following factors can become triggers in the occurrence of Perthes disease:
- Minor mechanical trauma (e.g., a bruise or sprain from jumping from a low height). Sometimes, the injury is so minor that it may go unnoticed. Sometimes, an awkward movement is all it takes.
- Inflammation of the hip joint (transient synovitis) in microbial and viral infections (flu, sore throat, sinusitis).
- Changing hormonal background in the transition age.
- Disorders of the metabolism of calcium, phosphorus, and other minerals involved in bone formation.
In some cases, a hereditary predisposition to the development of Perthes disease is detected, which may be due to a predisposition to myelodysplasia and genetically determined features of the hip joint's structure.
Classification
In traumatology and orthopedics, there are five stages of Perthes disease:
- Cessation of blood supply, formation of a focus of aseptic necrosis.
- Secondary depressed fracture of the femoral head in the fractured area.
- Dissolution of necrotic tissue accompanied by shortening of the femoral neck.
- Expansion of connective tissue at the site of necrosis.
- Replacement of connective tissue with new bone, fracture fusion.
The outcome of Perthes disease depends on the size and location of the necrosis site. If the area is small, full recovery is possible. In case of extensive destruction, the head disintegrates into several separate fragments and, after fusion, may acquire an irregular shape: flattened, protruding beyond the edge of the articular socket, etc. Violation of the normal anatomical relationship between the head and the acetabulum in such cases causes further aggravation of pathological changes: formation of contractures, limitation of support, and rapid development of severe coxarthrosis.
Symptoms of Perthes disease
In the early stages, there is non-intense, dull pain when walking. Usually, the pain is localized in the hip joint, but in some cases, there may be pain in the knee joint or throughout the leg. The child begins to noticeably limp, falls on the affected leg, or sticks it up. As a rule, during this period, the clinical manifestations are so weakly expressed that parents do not even think to consult an orthopedic doctor and explain the symptoms of the disease by a bruise, increased load, the consequence of an infectious disease, etc.
With further destruction of the head and the occurrence of an impression fracture, pain increases sharply, and lameness becomes pronounced. Soft tissues in the area of the joint swell. Movement limitations are revealed: the patient cannot turn the leg to the outside, and the hip joint's rotation, flexion, and extension are limited. Walking is difficult. There are autonomic disorders in the distal parts of the diseased limb - the foot is cold and pale, and its sweating is increased. There may be an increase in body temperature to subfebrile digits. Subsequently, the pain becomes less intense, and support on the leg is restored, but lameness and limitation of movement may persist. In some cases, shortening of the limb is detected. Over time, the clinic of progressive arthrosis appears.
Diagnosis
Radiography of the hip joint is the most important examination and crucial in diagnosing Perthes disease. If this disease is suspected, radiographs in several projections are performed. The radiologic picture depends on the stage and severity of the disease. There are various radiologic classifications, the most popular of which are the Catterall and Salter-Thompson classifications.
Catterall Classification:
- Group 1. Radiological signs of Perthes disease are weakly pronounced. There is a small defect in the central or subchondral zone. The femoral head has a normal configuration. The metaphysis has no changes; the fracture line is not defined.
- Group 2. The contours of the head are intact and destructive, and sclerotic changes are visible on the radiograph. There are signs of head fragmentation, and a forming sequestrum is detected.
- Group 3. The head is almost wholly affected and deformed. The fracture line is revealed.
- Group 4. The head is completely affected. The fracture line and acetabular changes are evident.
Salter-Thompson classification
- Group 1. Subchondral fracture is determined only on the X-ray in the Lauenstein projection.
- Group 2. The subchondral fracture is visible on all images, and the external border of the head is unchanged.
- Group 3. A subchondral fracture "engulfs" the outer part of the epiphysis.
- Group 4. The subchondral fracture extends to the entire epiphysis.
In doubtful cases in the first stage of the disease, an MRI of the hip joint is sometimes prescribed to assess the bone and soft tissue accurately.
Treatment of Perthes disease
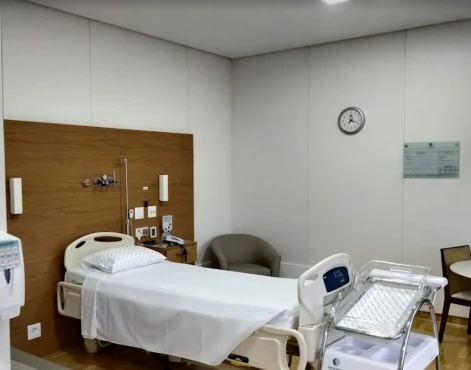
Children aged 2-6 years with mild symptoms and minimal changes on radiographs should be seen by a pediatric orthopedist; no special therapy is required. In other cases, patients are referred to the orthopedic department for treatment, followed by outpatient treatment. Conservative therapy is long-term, lasting at least a year (average 2.5 years, in severe cases up to 4 years). Treatment includes:
- Complete unloading of the limb.
- The application of skeletal traction, plaster casts, orthoses, and functional beds are used to prevent femoral head deformity.
- Improving blood supply to the joint using medication and non-medication methods.
- Stimulation of the processes of resorption of destroyed tissues and bone repair.
- Maintaining muscle tone.
Children with Perthes disease remain sedentary for a long time, which often provokes the emergence of excessive weight and the subsequent increase in the load on the joint. Therefore, all patients are prescribed a special diet to prevent obesity. In this case, the diet should be complete and rich in protein, fat-soluble vitamins, and calcium. Massage and special gymnastics complexes are used during the entire treatment period. When using skeletal traction and plaster casts that exclude the possibility of active movements, electrical stimulation of muscles is performed.
Children are prescribed angioprotectors and chondroprotectors orally and in intramuscular injections. Load on the leg is allowed only after radiologically confirmed fracture fusion. In the fourth stage, patients are allowed to perform active exercises, and in the fifth stage, a set of sports exercises is used to restore muscles and the volume of movement in the joint.
Surgery for Perthes disease is indicated in severe cases (severe deformity, hip subluxation) and only in children over six years of age. Usually, rotational transposition of the acetabulum, according to Salter, or corrective medializing osteotomy of the femur is performed. In the postoperative period, physical therapy, sports exercises, massage, chondroprotectors, and angioprotectors are prescribed.
Prognosis and prevention
With early detection and adequate treatment of pathology, the prognosis of Perthes disease is usually quite favorable, full recovery is possible. In severe cases, the outcome reveals deforming arthrosis. For people who have undergone this disease, regardless of the severity of the disease, it is recommended that excessive loads on the hip joint be excluded throughout life. Jumping, running, and lifting weights are contraindicated. Swimming and cycling are allowed. It is necessary to engage in therapeutic gymnastics regularly. Do not choose a job associated with heavy physical exertion or prolonged foot stay. It is necessary to undergo rehabilitation treatment in outpatient clinics and sanatoriums periodically.