Understanding Chronic Pain: A Comprehensive Exploration
This comprehensive article delves into the complexities of chronic pain, exploring its nature, causes, and the profound impact it has on individuals and society. It discusses the challenges in diagnosing chronic pain, outlines a range of treatment and management strategies, and emphasizes the importance of policy and advocacy. The article also looks forward to future directions in chronic pain research and treatment, offering hope and guidance for those affected by this persistent condition.
Introduction
Chronic pain is an often misunderstood and overlooked health condition, yet it affects a significant portion of the global population. Unlike acute pain, which is a normal sensation triggered in the nervous system to alert you to possible injury, chronic pain persists. Pain signals keep firing in the nervous system for weeks, months, or even years. This article seeks to shed light on the complexities of chronic pain, exploring its types, causes, impacts, and the various approaches to treatment and management.
Definition of Chronic Pain
At its core, chronic pain is pain that continues beyond the typical recovery time for an injury or illness. It's not just a prolonged version of acute pain; it's a distinct phenomenon that often involves changes in the nervous system and can occur even in the absence of an ongoing injury. Chronic pain can be continuous or intermittent, and its intensity may vary from mild to severe.
Prevalence and Significance
Chronic pain is a significant public health issue, affecting millions worldwide. According to various studies, it impacts more than 20% of the adult population, causing substantial disability and distress. It's a leading cause of long-term disability and is associated with numerous physical and mental health conditions, including depression and anxiety.
The Nature of Chronic Pain
Understanding the intrinsic characteristics of chronic pain is essential for effective management and empathy towards those affected by it. This section delves into the distinction between acute and chronic pain, explores various types of chronic pain, and discusses common conditions associated with it.
Difference Between Acute and Chronic Pain
Acute pain is a sudden, sharp sensation that serves as an alert to possible injury or disease, typically resolving as the underlying cause is treated. In contrast, chronic pain persists well beyond the expected period of healing, often lasting for months or even years. Unlike acute pain, chronic pain may not always have a clear cause and can continue even after the initial injury or illness has healed.
Types of Chronic Pain
Chronic pain manifests in various forms, each with unique characteristics:
- Neuropathic Pain: This type of pain arises from damage to the nerves or the nervous system and is often described as burning, shooting, or electric-like;
- Nociceptive Pain: Stemming from tissue damage (e.g., skin, muscles, bones), this pain is typically aching or throbbing in nature;
- Psychogenic Pain: Although less understood, this pain is linked to psychological factors and may not have a clear physical source.
Common Conditions Associated with Chronic Pain
Several medical conditions are frequently associated with chronic pain, each presenting its own set of challenges:
- Fibromyalgia: Characterized by widespread musculoskeletal pain, fibromyalgia often comes with fatigue, sleep, memory, and mood issues;
- Arthritis: This includes various types, such as osteoarthritis and rheumatoid arthritis, leading to chronic joint pain and stiffness;
- Migraines and Other Headaches: Chronic migraines or tension headaches can cause ongoing, debilitating head pain;
- Back Pain: One of the most common types of chronic pain, back pain can arise from a multitude of factors like muscle or ligament strain, bulging or ruptured disks, and skeletal irregularities.
Causes and Risk Factors
Identifying the underlying causes and risk factors of chronic pain is crucial for both prevention and effective treatment. Chronic pain can be the result of a variety of factors, often interlinked, affecting individuals differently.
Biological Factors
Biological influences play a significant role in the development of chronic pain. This includes:
- Age: Older adults are more susceptible to conditions like arthritis, which can lead to chronic pain;
- Sex: Certain types of chronic pain, such as fibromyalgia, are more prevalent in women;
- Injury: Past injuries, especially if not properly treated, can evolve into chronic pain conditions;
- Medical Conditions: Diseases like diabetes can lead to neuropathic pain, while autoimmune diseases can cause inflammatory pain.
Environmental and Lifestyle Factors
The environment and lifestyle choices can significantly influence the development of chronic pain:
- Occupational Hazards: Repetitive motion, heavy lifting, or prolonged sitting in the workplace can lead to chronic musculoskeletal pain;
- Lifestyle Choices: Lack of physical activity, poor diet, and smoking can increase the risk of developing chronic pain;
- Psychosocial Stressors: Chronic stress and traumatic events can exacerbate or trigger the onset of chronic pain.
Psychological Factors
The mind-body connection is vital in understanding chronic pain:
- Mental Health: Conditions like depression and anxiety can contribute to or exacerbate chronic pain;
- Coping Style: How individuals deal with stress and pain can impact their experience of chronic pain;
- Perception of Pain: The psychological interpretation of pain signals can influence the severity and persistence of chronic pain.
Genetics and Family History
Genetic predispositions play a role in the susceptibility to certain types of chronic pain:
- Genetic Factors: Certain genes can increase the risk of developing conditions like migraines or fibromyalgia;
- Family History: A family history of chronic pain conditions can be indicative of a higher risk in individuals.
Understanding these diverse factors is key to a comprehensive approach to treating and managing chronic pain.
The Impact of Chronic Pain
Chronic pain extends beyond mere physical discomfort, exerting a profound influence on various aspects of an individual's life and on society as a whole. This section explores the multifaceted impacts of chronic pain, emphasizing its far-reaching consequences.
Physical Effects
The persistent nature of chronic pain can lead to numerous physical complications:
- Reduced Mobility and Functionality: Chronic pain can limit an individual's ability to move freely, leading to decreased mobility and impaired physical function;
- Sleep Disturbances: Many individuals with chronic pain experience difficulties with sleep, which can exacerbate other health issues;
- Weakened Immune System: Chronic pain and associated stress can weaken the immune system, making the body more susceptible to infections and illnesses;
- Increased Risk of Other Physical Conditions: Conditions such as cardiovascular disease and obesity are often associated with chronic pain, partly due to reduced physical activity.
Psychological Effects
The psychological impact of chronic pain is as significant as its physical effects:
- Depression and Anxiety: The constant presence of pain can lead to feelings of hopelessness and anxiety, significantly affecting mental health;
- Cognitive Impairment: Chronic pain can impair cognitive functions, including memory, attention, and decision-making;
- Emotional Strain: Living with persistent pain can lead to emotional exhaustion, irritability, and a reduced capacity to cope with stress.
Social and Economic Impact
Chronic pain also has broader social and economic implications:
- Impact on Employment and Productivity: Chronic pain can lead to reduced productivity at work, frequent absences, or even disability, impacting an individual's career and financial stability;
- Strain on Relationships: The burden of chronic pain can affect relationships, leading to social isolation or strained family dynamics;
- Healthcare Costs: The ongoing need for medical care, including doctor visits, medications, and therapies, can lead to significant healthcare expenses;
- Societal Costs: At a larger scale, chronic pain contributes to substantial economic costs due to lost workdays, healthcare expenditures, and disability benefits.
Diagnosis and Assessment
Diagnosing and assessing chronic pain poses significant challenges due to its subjective nature and the variety of underlying causes. This section focuses on these challenges and the methods used to evaluate chronic pain effectively.
Challenges in Diagnosing Chronic Pain
The diagnosis of chronic pain is often a complex and nuanced process, involving several challenges:
- Subjectivity of Pain: Pain is a subjective experience, varying greatly from person to person, making it difficult to quantify and assess objectively;
- Lack of Objective Markers: Unlike other medical conditions, there are no specific tests that can conclusively diagnose chronic pain;
- Communication Barriers: Patients may have difficulty articulating the nature and extent of their pain, and doctors might misinterpret these descriptions;
- Variable Manifestations: Chronic pain can present differently in individuals, and symptoms may fluctuate over time.
Tools and Techniques for Assessment
Despite these challenges, several tools and techniques are employed to diagnose and assess chronic pain:
- Pain Scales and Questionnaires: Tools like the Visual Analog Scale (VAS), Numeric Rating Scale (NRS), and the McGill Pain Questionnaire help in quantifying pain levels and understanding its impact on daily activities;
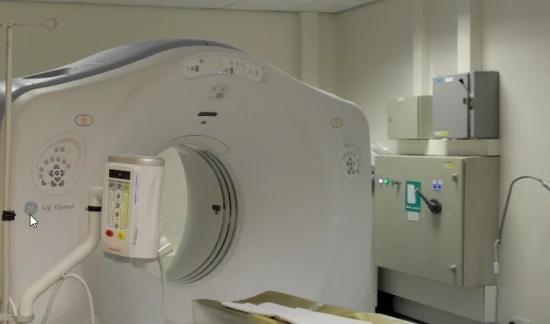
- Medical Imaging: While not able to detect pain directly, imaging techniques like X-rays, MRIs, and CT scans can help identify underlying physical conditions that might be contributing to the pain;
- Physical Examination: A thorough physical examination can provide insights into pain sources and rule out other potential causes;
- Pain Diaries: Patients may be asked to keep a pain diary, documenting the intensity of pain, triggers, and its impact on their daily life;
- Psychological Assessment: Given the interplay between mental health and chronic pain, psychological evaluations can be crucial in understanding the patient's experience of pain.
Treatment and Management Strategies
Effective treatment and management of chronic pain often require a multifaceted approach, tailored to the individual's specific needs and the nature of their pain. This section explores various strategies, ranging from medication to lifestyle modifications, that are used to manage chronic pain.
Medications
Medications are a common component of chronic pain management, but they must be carefully chosen and monitored due to potential side effects and the risk of dependency.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and acetaminophen can be effective for mild to moderate pain;
- Prescription Medications: For more severe pain, doctors may prescribe stronger painkillers, including opioids (with strict monitoring), muscle relaxants, or antidepressants, which can also help alleviate pain;
- Topical Medications: Creams and ointments containing lidocaine or capsaicin can be used for localized pain relief.
Non-Pharmacological Approaches
In many cases, non-pharmacological treatments can be as effective as medications and are essential for a holistic approach to pain management.
- Physical Therapy: Tailored exercise and stretching programs can improve strength and flexibility, reducing pain;
- Psychological Therapies: Cognitive-behavioral therapy (CBT) and other forms of psychotherapy can help patients manage the emotional aspects of chronic pain;
- Alternative Therapies: Acupuncture, chiropractic care, and massage therapy are often used as complementary treatments for pain relief.
Lifestyle Modifications
Lifestyle changes play a critical role in managing chronic pain and improving overall well-being.
- Diet and Nutrition: A balanced diet, including anti-inflammatory foods and those supporting liver health, can aid in reducing pain and improving medication management. Foods such as leafy greens, garlic, nuts, and fatty fish are beneficial for liver health. Avoiding excessive alcohol and processed foods also supports liver function;
- Exercise: Regular, gentle exercise like walking, swimming, or yoga can help keep the body active and reduce pain;
- Stress Management: Techniques like meditation, deep breathing, and relaxation exercises can help in managing stress, which can exacerbate pain. Managing stress also supports liver health, as chronic stress can impact bodily systems;
- Hydration and Detoxification: Adequate hydration and a diet rich in antioxidants can support the body's natural detoxification processes, including liver function;
- Avoiding Harmful Substances: Reducing intake of substances harmful to the liver, such as certain medications, alcohol, and recreational drugs, is crucial for overall body health and pain management.
Emerging Treatments and Research
The field of pain management is continuously evolving, with new treatments and research providing hope for chronic pain sufferers.
- Neuromodulation Techniques: Treatments like spinal cord stimulation or transcranial magnetic stimulation are showing promise in managing certain types of pain;
- Regenerative Medicine: Techniques like stem cell therapy and platelet-rich plasma (PRP) injections are being explored for their potential in treating chronic pain;
- Personalized Medicine: Advances in understanding genetic and biochemical aspects of pain could lead to more targeted and effective treatment strategies.
Living with Chronic Pain
Living with chronic pain is a daily challenge that affects not only the physical state but also the emotional and social wellbeing of individuals. This section discusses strategies for coping with chronic pain, the importance of support systems, and shares insights from patient stories and experiences.
Coping Strategies
Developing effective coping strategies is crucial for individuals living with chronic pain. These strategies can help manage pain levels and improve overall quality of life.
- Pain Management Skills: Learning techniques to manage pain, such as pacing activities, using heat or cold therapy, and practicing mindfulness, can be beneficial;
- Cognitive Behavioral Therapy (CBT): This type of therapy helps in changing the thought patterns associated with pain, leading to better pain management;
- Relaxation Techniques: Practices like deep breathing, meditation, and yoga can help reduce stress and alleviate pain;
- Hobbies and Interests: Engaging in hobbies or activities that bring joy and fulfillment can be a helpful distraction from pain.
Support Systems and Resources
Having a robust support system is vital for individuals dealing with chronic pain.
- Healthcare Team: Regular consultations with healthcare providers, including doctors, physical therapists, and mental health professionals, are essential for effective pain management;
- Support Groups: Joining support groups, either in person or online, can provide a sense of community and shared understanding;
- Family and Friends: Support from family and friends is crucial for emotional support and practical help in managing daily activities;
- Educational Resources: Access to accurate information about chronic pain can empower individuals to understand and manage their condition better.
Patient Stories and Experiences
Sharing and listening to personal stories and experiences can be incredibly powerful for people living with chronic pain.
- Personal Narratives: These stories can provide insights, hope, and a sense of connection to others facing similar challenges;
- Learning from Others: Understanding how others cope with their pain can offer new strategies and perspectives for managing one’s own pain;
- Raising Awareness: Patient stories help in raising awareness about the realities of living with chronic pain, promoting greater empathy and understanding.
The journey of living with chronic pain is unique to each individual, but through effective coping strategies, strong support systems, and shared experiences, it can become more manageable.
Policy and Advocacy
Addressing chronic pain not only involves individual management strategies but also requires broader policy initiatives and advocacy efforts. This section highlights the role of public awareness, healthcare policies, and community involvement in improving the lives of those suffering from chronic pain.
Public Awareness and Education
Raising public awareness about chronic pain is crucial in combating misconceptions and stigma associated with this condition.
- Awareness Campaigns: Campaigns aimed at educating the public about the nature of chronic pain can help in reducing stigma and promoting empathy;
- Educational Programs: Implementing educational programs in schools, workplaces, and community centers can aid in early recognition and proper management of chronic pain.
Healthcare Policies and Access to Treatment
Effective healthcare policies are essential to ensure that individuals with chronic pain have access to the care and resources they need.
- Access to Care: Advocacy for policies that improve access to comprehensive pain management services, including mental health support, physical therapy, and alternative treatments;
- Insurance Coverage: Working towards broader insurance coverage for various pain management therapies;
- Research Funding: Advocating for increased funding for chronic pain research to develop new and more effective treatment methods.
Advocacy Groups and Community Involvement
Active involvement of advocacy groups and communities plays a pivotal role in driving change and supporting those with chronic pain.
- Patient Advocacy Groups: These groups provide a platform for individuals with chronic pain to voice their needs and concerns, influencing policy decisions;
- Community Support Initiatives: Local community initiatives can offer practical support, such as transportation to medical appointments or assistance with daily tasks;
- Partnerships with Healthcare Providers: Collaborating with healthcare providers and institutions to improve care models and treatment approaches for chronic pain management.
Future Directions
The field of chronic pain management is continually evolving, with ongoing research and technological advancements opening new avenues for understanding and treating this complex condition. This section explores the potential future directions in chronic pain research, treatment, and technology.
Advances in Research
Continued research is crucial for gaining deeper insights into the mechanisms of chronic pain, which can lead to more effective treatments.
- Understanding Pain Mechanisms: Research aimed at unraveling the biological and neurological processes underlying chronic pain could lead to more targeted therapies;
- Personalized Medicine: Developing treatments tailored to individual genetic, environmental, and lifestyle factors holds promise for more effective pain management;
- Epidemiological Studies: Large-scale studies examining the prevalence and impact of chronic pain can inform public health strategies and policy-making.
Potential Breakthroughs in Treatment
The future of chronic pain treatment may see groundbreaking developments, offering hope to those who suffer from persistent pain.
- New Medications: The development of new pharmaceuticals with fewer side effects and lower risks of dependency;
- Regenerative Medicine: Exploring the potential of stem cell therapy and tissue engineering in repairing damaged nerves or tissues causing pain;
- Alternative and Complementary Therapies: Greater acceptance and integration of alternative therapies, such as acupuncture and herbal remedies, into mainstream pain management.
The Role of Technology in Managing Chronic Pain
Technology is set to play a significant role in the future of chronic pain management.
- Wearable Devices: Advanced wearable technology for monitoring pain levels and physiological responses, enabling more precise pain management;
- Telemedicine: The expansion of telemedicine services for pain management, making it more accessible to those in remote or underserved areas;
- Virtual Reality (VR) and Augmented Reality (AR): Using VR and AR for pain distraction therapy and rehabilitation exercises;
- Artificial Intelligence (AI): The application of AI in diagnosing pain conditions, predicting treatment outcomes, and personalizing pain management plans.
Conclusion
This article has provided an in-depth exploration of chronic pain, a condition that impacts millions worldwide. From understanding its nature and causes to exploring various treatment strategies and the importance of policy and advocacy, our journey through the complex world of chronic pain has been comprehensive.
Clinical physiology of pain, pathophysiology of pain
Pain and its mechanisms
The purpose of medicine is to preserve and restore health and alleviate suffering. Understanding the pathophysiology of pain (mechanisms of its development) is necessary to achieve both of these goals. Pain is perceived by us as a signal of the disease, it is the most common symptom that attracts the attention of a doctor. Below we will analyze the mechanisms of pain, and also touch on its features in oncology.
What is pain and does it always occur only when a tissue or organ is damaged?
According to the International Association for the Study of Pain (IASP), “pain is an unpleasant sensation and emotional experience associated with or described in terms of actual or potential tissue damage.” From this definition it follows that pain can occur not only with tissue damage, but also in its absence. Thus, a person's perception of pain, their emotional reaction and behavior may not coincide with the degree of damage.
Does pain have a function?
The function of the pain perception system is to protect the body and maintain a constancy of the internal environment (homeostasis). Often the localization of pain indicates the place of development of the pathological process. The nature of the pain syndrome, its dynamics over time and the place of occurrence provide important diagnostic clues for the doctor.
How does pain occur?
This symptom occurs with suprathreshold irritation of pain receptors (nociceptors). The latter are free nerve endings and are widely distributed in the surface layers of the skin, internal organs, vessel walls, periosteum, etc. When nociceptors are stimulated, sodium and potassium ions are released from them, as well as anti-inflammatory molecules: bradykinin, histamine, serotonin and prostaglandins.
Pain is caused by three types of stimuli:
- mechanical (trauma, compression);
- thermal (burn);
- chemical (action of endogenous molecules, such as bradykinin, serotonin, histamine, acetylcholine, proteolytic enzymes, etc.).
Can a person get used to pain?
Pain receptors are not adaptable. On the contrary, in a number of cases, against the background of long-acting pain stimulation, the excitation of pain fibers gradually increases. This process is especially characteristic of slow, aching or accompanied by nausea pain and is called hyperalgesia.
How is the pain impulse conducted?
Pain receptors use two pathways (fast and slow) to transmit impulses to the corresponding parts of the central nervous system. Signals of rapid (acute) pain arise under the action of mechanical and thermal factors and are transmitted at a speed of 6 to 30 m/s. Slow (chronic) pain is provoked in most cases by chemical stimuli (less often by long-acting mechanical and thermal stimuli) and is transmitted at a speed of 0.5–2 m/s along type C fibers.
The process of pain in general can be described as follows. First, sensitive neurons transform the damaging effect into electrical activity. Then impulses are conducted through the system of sensitive neurons through the tissues of the spinal cord to the thalamocortical zone of the brain. Further, nociceptive signals in the structures of the spinal cord are modified and perceived by a specific patient with his personal characteristics - this is how pain sensations are formed.
Depending on the origin (etiology) and pathogenesis (development mechanisms), pain syndromes are divided into:
- somatogenic (nociceptive pain);
- neurogenic (neuropathic pain);
- psychogenic (idiopathic) pain sensations are also distinguished.
Nociceptive pain
Occurs as a result of excitation of nociceptors in tissues: bones, internal organs, joints and muscles. It is characterized by intermittent or constant localized pains that are described as aching, stitching or throbbing.
The cause of visceral (pertaining to the internal organs) pain can be any stimulus that excites pain nerve endings in the internal organs. These incentives include:
- ischemia (impaired flow of oxygen-rich blood to the organ);
- chemical irritation of the surfaces of internal organs (for example, when pancreatic enzymes enter the bloodstream);
- spasm of smooth muscles (pain syndrome associated with mechanical stimulation of painful nerve endings);
- overstretching of hollow organs (painfulness in this case probably occurs due to the strong tension of the tissues themselves, blood vessels, as well as the associated ischemia);
- tension of the connective tissue around or inside the organs.
Virtually any pain in the chest and abdominal cavities is transmitted along fine type C pain fibers and, therefore, can only be felt as chronic, burning, excruciating pain. It is also accompanied by motor and autonomic reflexes, such as nausea and vomiting. Hypersensitive areas to damaging factors are called zones of hyperalgesia.
Neuropathic pain
The defeat of the peripheral or central nociceptive pathways usually leads to loss or deterioration of pain sensitivity. Paradoxically, damage or dysfunction to these pathways can also cause pain. For example, damage to peripheral nerves and afferent fibers, as occurs in diabetic neuropathy or herpes zoster, can lead to pain.
Pain may also be associated with damage to the central nervous system, for example after an injury. Such neuropathic pain is often severe and usually resistant to standard pain management. Neuropathic pain is typically characterized by an unusual burning, tingling, or electric shock sensation and can be triggered by very light touch.
Hypersensitivity is due to an increase in the number of sodium channels in the damaged nerve fiber. Damaged primary afferent fibers and pain-transmitting neurons in the spinal cord can also become spontaneously active in pathology.
Psychogenic or idiopathic pain
The term "idiopathic pain" is often used in place of "psychogenic pain" and is more appropriate as it encompasses a wide range of poorly understood pain conditions such as myofascial pain syndrome and somatic pain disorder.
Also, this type of pain may be part of a hysterical reaction or occur with psychopathology (for example, hallucinations or depression).
Are there any organs that are insensitive to pain?
Some tissues and organs in our body are completely insensitive to any type of pain. These include, for example, the liver and alveoli of the lungs. However, the liver capsule and bile ducts are very sensitive to pain stimuli, which can occur both in direct trauma and in sprains. The bronchi and pleura also have nociceptors.
Does pain always reflect the location of the injury?
In some cases, such as myocardial infarction, pain may radiate to the arm, upper jaw, or abdomen, and the patient may not realize that he has a heart problem that requires immediate medical attention.
What symptoms may accompany pain?
Any pain of moderate or high intensity is accompanied by anxiety and the desire to avoid or stop this feeling. This illustrates the duality of pain, which is both sensation and emotion. In acute pain syndrome, behavioral arousal and a reaction to stress occur: blood pressure and cortisol levels in the blood plasma increase, heart rate and pupil diameter increase. In addition, local muscle contraction (eg, limb flexion, abdominal wall rigidity) is often present.
Pain and cancer
An unpleasant sensory and emotional experience of pain is reported by 50 to 90% of people diagnosed with cancer. Pain in oncology reduces the overall quality of life due to adverse effects on the patient's emotions, cognitive functions, daily activities, family relationships and other social areas.
Pain is either directly related to the development and progression of cancer, or associated with diagnostic and therapeutic procedures and interventions, such as during biopsy or after surgery. Anticancer treatments, including chemotherapy, hormonal and steroid therapy, also cause acute pain. The mechanisms of cancer pain are complex and may combine nociceptive and neuropathic pain.
Summary
Depending on the pathophysiology, pain syndromes are divided into somatogenic (nociceptive pain), neurogenic (neuropathic pain) and idiopathic (psychogenic). There are tissues that are insensitive to pain.
Cancer pain can result from all cancer treatments, including surgery, radiation, hormone therapy, and chemotherapy. Regardless of the origin of the pain, the doctor must take appropriate measures for rapid and effective pain relief.
References:
- Harrison`s Principles of Internal Medicine 19/E (Vol.1). Dennis Kasper, Anthony Fauci, Stephen Hauseret all. McGraw-HillEducation 2015 ISBN: 0071802134 ISBN-13(EAN): 9780071802130.
- Guyton, A.K. Medical physiology / A.K. Guyton, J.E. Hall / Per. from English; Ed. IN AND. Kobrin. - M .: Logosphere, 2008. - 1296 p .: ill. : 21.1 cm - ISBN 978-5-98657-013-6.
- Russo, M. M., & Sundaramurthi, T. (2019). An Overview of Cancer Pain: Epidemiology and Pathophysiology. Seminars in Oncology Nursing. doi:10.1016/j.soncn.2019.04.002.
- Anwar, K. (2016). Pathophysiology of pain. Disease-a-Month, 62(9), 324–329. doi:10.1016/j.disamonth.2016.05.015.
- Nazarov IP Pathophysiology of pain syndromes, principles of treatment (message 1) // Siberian Medical Review. 2006. No. 4.