Navigating Benign Liver Tumors: A Guide to Diagnosis, Treatment, and Prevention Strategies
Benign liver tumors are non-cancerous growths in the liver. Unlike malignant liver tumors, they don't spread to other parts of the body and are generally considered less serious. However, they can still cause health issues and require medical attention. Understanding these tumors is key to managing and preventing complications.
The three most common types of benign liver tumors are:
- Hepatic hemangioma;
- Hepatocellular adenoma;
- Focal nodular hyperplasia.
Hepatic hemangioma
Hemangiomas are the most common type of benign liver tumors, characterized primarily by their vascular nature. They consist of a tangle of blood vessels and are often discovered incidentally during imaging tests for other conditions. Hemangiomas can occur in individuals of any age, but they are more frequently diagnosed in adults, particularly in women.
Characteristics
- Appearance: Typically, hemangiomas are small, ranging from a few millimeters to a few centimeters in size. They are usually solitary but can be multiple in some cases.
- Growth: Generally, hemangiomas grow slowly and remain asymptomatic. They rarely increase in size or become symptomatic, which distinguishes them from more aggressive types of liver tumors.
Risk Factors
- Gender: Women are more likely to develop hemangiomas than men, potentially due to hormonal influences.
- Age: Although they can be present at any age, hemangiomas are most commonly identified in adults between 30 and 50 years of age.
- Hormones: Hormonal factors, including the use of oral contraceptives, have been suggested as a possible risk factor, although the evidence is not definitive.
Symptoms
Most liver hemangiomas do not cause symptoms and are often discovered during imaging studies performed for unrelated reasons. When symptoms do occur, they may include:
- Abdominal discomfort or pain, particularly in the upper right abdomen.
- Feeling of fullness after eating a small amount of food.
- Nausea or bloating.
Diagnosis
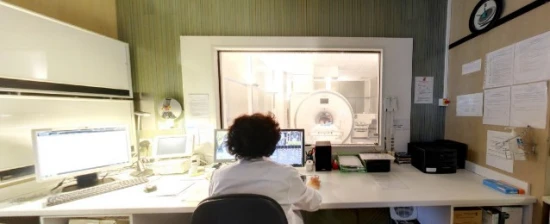
Hemangiomas are typically diagnosed through imaging studies, including:
- Ultrasound: Often the first imaging technique used when a liver abnormality is suspected.
- Computed Tomography (CT) Scan: Provides detailed images and can help in distinguishing hemangiomas from other types of liver lesions.
- Magnetic Resonance Imaging (MRI): Offers high-resolution images and is particularly effective in diagnosing liver hemangiomas.
Treatment
In most cases, treatment is not necessary for liver hemangiomas, especially if they are small and asymptomatic. The primary approach is regular monitoring to check for any changes in size or appearance. In rare cases where hemangiomas are large or symptomatic, treatment options may include:
- Surgical Removal: Indicated if the hemangioma causes significant symptoms or complications.
- Embolization: A procedure to block the blood supply to the hemangioma, causing it to shrink.
Complications
While complications from liver hemangiomas are rare, they can include:
- Rupture: Although extremely rare, a ruptured hemangioma can cause internal bleeding.
- Kasabach-Merritt Syndrome: A rare complication involving a large hemangioma that leads to blood clotting issues.
Hepatocellular Adenoma
Hepatocellular adenoma (HCA) is a rare type of benign liver tumor that primarily affects the liver's functioning cells, known as hepatocytes. It's more commonly found in women and has a strong association with hormonal factors. While hepatocellular adenomas are benign, they can have significant health implications due to their potential for complications.
Characteristics
- Composition: HCAs are composed of abnormal liver cells and often lack the normal architecture of the liver, including bile ducts and portal tracts.
- Appearance: These tumors can vary in size, and while they are usually solitary, multiple adenomas can also occur.
Risk Factors
- Gender and Hormones: Predominantly affects women, particularly those using oral contraceptives or during pregnancy, due to hormonal influences.
- Anabolic Steroids: Use of anabolic steroids can also increase the risk.
- Metabolic Disorders: Certain metabolic disorders like glycogen storage diseases can predispose individuals to HCAs.
Symptoms
- Asymptomatic Nature: Many HCAs do not cause symptoms and are often discovered incidentally during imaging for other reasons.
- Potential Symptoms: When symptoms do occur, they can include abdominal pain or fullness, particularly in the upper right quadrant of the abdomen.
Diagnosis
- Imaging Studies: Ultrasound, CT scans, and MRI are commonly used to identify and characterize the tumor. These imaging tests can help differentiate HCAs from other liver lesions.
- Biopsy: Sometimes, a biopsy is necessary to confirm the diagnosis, particularly if the imaging is inconclusive.
Treatment
- Monitoring: Small, asymptomatic HCAs might only require regular monitoring with imaging.
- Hormonal Contraceptives: Women with HCAs are often advised to stop using oral contraceptives or other hormonal treatments, as these can influence the growth of the adenoma.
- Surgical Removal: Surgery may be recommended for large adenomas (typically those over 5 cm), symptomatic adenomas, or if there is a concern about malignancy.
Complications
- Hemorrhage: One of the most significant risks is bleeding within the tumor or into the abdominal cavity, which can be life-threatening.
- Malignant Transformation: Although rare, HCAs can transform into hepatocellular carcinoma, a type of liver cancer.
Prevention
- Contraceptive Use: Women at risk for HCAs may need to consider non-hormonal forms of contraception.
- Regular Monitoring: For those with risk factors like metabolic disorders, regular liver imaging can help in early detection.
Focal Nodular Hyperplasia (FNH)
Focal Nodular Hyperplasia (FNH) is a benign liver lesion, typically considered the second most common type of benign liver tumor after hemangiomas. FNH is composed of a mixture of various cell types found in the liver, and it is usually discovered incidentally during imaging studies for other medical reasons.
Characteristics
- Composition: FNH is characterized by a mixture of hepatocytes (liver cells), Kupffer cells (a type of immune cell in the liver), and fibrous tissue.
- Appearance: On imaging, FNH usually appears as a well-defined, solitary mass with a central scar, although the scar is not always present.
- Growth: FNH lesions are generally stable in size and do not tend to grow or shrink significantly over time.
Risk Factors
- Gender and Age: FNH is more commonly diagnosed in women, particularly during their reproductive years, although it can occur in both genders and at any age.
- Hormonal Influence: Unlike hepatic adenomas, FNH is not strongly linked to hormonal factors, such as oral contraceptive use.
Symptoms
- Asymptomatic Nature: Most individuals with FNH do not experience any symptoms, and the lesions are usually found incidentally during imaging for unrelated reasons.
- Possible Symptoms: On rare occasions, particularly with larger lesions, individuals may experience discomfort or pain in the upper abdomen, a feeling of fullness, or other nonspecific gastrointestinal symptoms.
Diagnosis
- Imaging Studies: FNH is typically diagnosed through imaging techniques such as ultrasound, CT scans, or MRI. These modalities can help differentiate FNH from other liver lesions.
- Central Scar Feature: The presence of a central scar seen in imaging studies can be suggestive of FNH, although it's not present in all cases.
Treatment
- Monitoring: Since FNH lesions are benign and usually asymptomatic, they typically do not require treatment. Regular monitoring with imaging may be recommended to ensure the lesion remains stable.
- Surgery: Surgical intervention is rarely required and is usually considered only if the lesion causes significant symptoms or if there's uncertainty in the diagnosis.
Complications
Rare Occurrences: FNH is not known to rupture or bleed and does not have malignant potential. Complications are extremely rare.
Prevention
No Specific Prevention. Since the exact cause of FNH is unclear and it is not linked to lifestyle factors, there are no specific preventive measures.
Conclusion
Benign liver tumors, though not life-threatening, require careful monitoring and management due to their potential to cause discomfort and other complications. Understanding the types, risk factors, and treatment options is crucial for individuals diagnosed with these tumors. With ongoing research and advancements in medical treatments, the outlook for managing benign liver tumors continues to improve, offering effective and less invasive options for those affected. Regular medical check-ups and maintaining a healthy lifestyle are key preventive strategies to ensure liver health and early detection of any abnormalities.