Definition
Brain astrocytoma is a primary intracerebral neuroepithelial (glial) tumor originating from stellate cells (astrocytes). Astrocytoma of the brain can have varying degrees of malignancy. Its manifestations depend on the localization and are divided into general (weakness, loss of appetite, headaches) and focal (hemiparesis, hemihypesthesia, coordination disorders, hallucinations, speech disorders, behavioral changes). Brain astrocytoma is diagnosed based on clinical data, CT, MRI, and histological examination of tumor tissue. Treatment of brain astrocytoma is usually a combination of several methods: surgery or radiosurgery, radiation, and chemotherapy.
General information
Astrocytoma of the brain is the most common type of glial tumor. Approximately half of all brain gliomas are represented by astrocytomas. Brain astrocytoma can occur at any age. Most often, brain astrocytoma is noted in men between 20 and 50 years of age. In adults, the most characteristic localization of brain astrocytoma is the white matter of the hemispheres (cerebral hemispheric tumor); in children, lesions of the cerebellum and brain stem are more common. The optic nerve is rarely affected in children (chiasmatic glioma and optic nerve glioma).
Etiology of a brain astrocytoma
Astrocytoma results from tumorigenesis of astrocytes, glial cells that have a star shape, for which they are also called star cells. Until recently, astrocytes were thought to have an auxiliary supportive function in relation to CNS neurons. However, recent studies in the field of neurophysiology and neuroscience have shown that astrocytes perform a protective function, preventing injury to neurons and absorbing excessive chemicals formed as a result of their activity. They provide nutrition for neurons and participate in the regulation of the blood-brain barrier and cerebral blood flow.
Precise data on the factors that provoke tumor transformation of astrocytes have yet to be available. Presumably, the role of the trigger mechanism, as a result of which brain astrocytoma develops, is played by excessive radiation, chronic exposure to harmful chemicals, and oncogenic viruses. A significant role is also attributed to the hereditary factor since patients with brain astrocytoma have been found to have genetic defects in the TP53 gene.
Classification
Brain astrocytoma can be “normal” or “specific,” depending on the structure of its constituent cells. The first group includes fibrillary, protoplasmic, and gemistocytic brain astrocytomas. The “special” group includes pilocytic, subependymal (glomerular), and microcystic cerebellar astrocytoma of the brain.
According to the WHO classification, brain astrocytomas are subdivided according to the degree of malignancy. Grade I malignancy belongs to the “special” brain astrocytoma – pilocytic. II degree of malignancy is characteristic of “ordinary” benign astrocytomas, such as fibrillary. To the III degree of malignancy belongs anaplastic astrocytoma of the brain, to the IV degree – glioblastoma. Glioblastoma and anaplastic astrocytoma account for about 60% of brain tumors, while highly differentiated (benign) astrocytomas account for only 10%.
Symptoms of astrocytoma
Clinical manifestations accompanied by astrocytoma of the brain can be divided into general, noted at any location of the tumor, and local or focal, depending on the localization of the process.
Common symptoms of astrocytoma are related to the resulting increase in intracranial pressure, irritative effects, and toxic effects of metabolic products of tumor cells. Common manifestations of brain astrocytoma include constant headaches, lack of appetite, nausea, vomiting, double vision and/or foggy eyes, dizziness, mood changes, asthenia, decreased ability to concentrate, and memory impairment. Epileptic seizures are possible. Often, the first manifestations of cerebral astrocytoma are generally nonspecific. Over time, depending on the degree of malignancy of astrocytoma, there is a slow or rapid progression of symptoms with the appearance of neurological deficit, indicating the focal nature of the pathological process.
Focal symptoms of cerebral astrocytoma are caused by the destruction and compression of cerebral structures located near the tumor. Hemispheric brain astrocytomas are characterized by decreased sensation (hemihypesthesia) and muscle weakness (hemiparesis) in the arm and leg on the side of the body opposite to the affected hemisphere. Tumor lesions of the cerebellum are characterized by impaired stability in standing and walking and problems with movement coordination.
The location of brain astrocytoma in the frontal lobe is characterized by inertness, sharply expressed general weakness, apathy, decreased motivation, bouts of mental agitation and aggressiveness, and deterioration of memory and intellectual abilities. People around such patients note changes and oddities in their behavior. When localization of astrocytoma in the temporal lobe, there are speech disorders, memory disorders, and hallucinations of different natures: olfactory, auditory, and gustatory. Visual hallucinations are characteristic of astrocytoma located on the border of the temporal lobe with the occipital lobe. If the brain astrocytoma is localized in the occipital lobe, then along with visual hallucinations, it is accompanied by various visual disturbances. Dark brain astrocytoma causes a disorder of written speech and acceptable motor disorders.
Diagnosis of astrocytoma of the brain
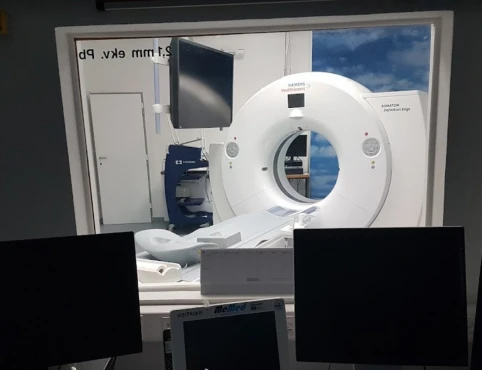
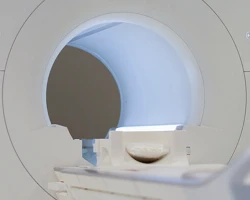
A neurologist, neurosurgeon, ophthalmologist, and otolaryngologist perform clinical examinations of patients. These examinations include neurologic examination, ophthalmologic examination (determination of visual acuity, visual field examination, ophthalmoscopy), threshold audiometry, examination of the vestibular apparatus, and mental status. Primary instrumental examination of patients with cerebral astrocytoma can reveal increased intracranial pressure according to echoencephalography and the presence of paroxysmal activity according to electroencephalography. Detection of focal symptomatology during neurological examination indicates CT and MRI of the brain.
Brain astrocytoma can also be detected by angiography. Histological examination allows for the establishment of a precise diagnosis and determination of the tumor’s degree of malignancy. Histologic material can be obtained during stereotactic biopsy or intraoperatively (to decide the extent of surgical intervention).
Treatment of astrocytoma of the brain
Depending on the degree of differentiation of astrocytoma of the brain, its treatment is carried out by one or more of these methods: surgical, chemotherapeutic, radiosurgical, and radiation therapy.
Stereotactic radiosurgical removal is only possible for small tumors (up to 3 cm) and is performed under tomographic control using a stereotactic frame placed on the patient’s head. In brain astrocytoma, this method can be used only in rare cases of benign course and limited tumor growth. The extent of surgical intervention by cranial trepanation depends on the nature of the astrocytoma growth. Often, due to diffuse tumor growth into the surrounding brain tissue, its radical surgical treatment is impossible. In such cases, palliative surgery to reduce the size of the tumor or shunt surgery to reduce hydrocephalus may be performed.
Radiation therapy for brain astrocytoma involves repeated (10 to 30 sessions) external irradiation of the affected area. Chemotherapy, using cytostatics, is carried out with oral drugs and intravenous injections. It is favored in children with brain astrocytoma. Recently, new chemotherapeutic drugs have been actively developed that can selectively affect tumor cells without damaging healthy cells.
Prognosis of astrocytoma of the brain
The unfavorable prognosis of cerebral astrocytoma is associated with its predominantly high degree of malignancy, frequent transition of a less malignant form to a more malignant form, and almost inevitable recurrence. In persons of young age, a more common and malignant course of astrocytomas is observed. The most favorable prognosis is if the brain astrocytoma has I degree of malignancy, but even in this case, the patient’s life expectancy does not exceed five years. For grade III-IV astrocytoma, this time is, on average, one year.