Introduction: Basics of Basal Cell Carcinoma (BCC)
Basal cell skin cancer is the most common skin cancer. If caught early, it is easily treatable. This is because it grows very slowly.
Basal cell skin cancer is caused by exposure to ultraviolet (UV) radiation. UV radiation from the sun or indoor tanning beds causes damage to basal cells found in the outermost layer of skin (epidermis). UV radiation has been found to damage the DNA (deoxyribonucleic acid) inside skin cells. DNA is the chemical in our cells that make up our genes. DNA controls how our cells develop, grow, and function.
Basal cell skin cancer usually develops in areas exposed to the sun, including the face, head, and neck. But it can occur anywhere on the body.
Basal cell skin cancer can cause a lot of damage to the patient's skin. It may involve areas of soft tissue, cartilage, and bone. People can sometimes lose part of an ear or nose. On a positive note, basal skin cancer rarely metastasizes. Metastasis refers to cancer spreading from an initial site to a different or secondary site.
Sometimes, people go to the doctor because they have a sore or a cut from shaving that just won't heal, which turns out to be a basal cell cancer. A simple rule of thumb is that most shaving cuts heal within a week or so. Look out for any new, changing, or unusual skin growths. Skin cancer is more accessible to treat and cure when it is caught early.
Introduction: Basics of Squamous Cell Carcinoma (SCC)
Squamous cell skin cancer is a common skin cancer, especially in fair-skinned people. It is the second most common type of skin cancer after basal cell carcinoma. The third type—melanoma—is much less common than the other types but can be more aggressive.
Because they do not behave like melanoma, basal cell and squamous cell skin cancers are often referred to as non-melanoma skin cancers or keratinocyte carcinomas.
Cancer that starts in a squamous cell is called a squamous cell carcinoma. Squamous cells are found in the top layer of the skin. They can also be found in other body areas, such as the lungs, thyroid, and esophagus. These types are treated differently than cutaneous squamous cell carcinoma. Squamous cell skin cancers often begin as scaly patches on the skin that can become solid and distorted. This cancer is also called cutaneous squamous cell carcinoma (CSCC). Squamous cell skin cancer can form in old wounds, burns, or scars. This is called Marjolin's ulcer and can be harder to treat. Also, patients with actinic keratoses, a weakened immune system, or specific genetic syndromes such as epidermolysis bullosa are more predisposed to CSCC development than others.
Algorithm of diagnosis
What evaluations do non-melanoma skin cancer patients undergo to identify the best treatment strategy?
- Physical examination: check the patient's temperature, blood pressure, pulse, breathing rate, body weight, enlarged lymph nodes in the neck, underarms, and groin.
- Close examinations of skin lesions and a complete skin exam: a head-to-toe skin exam that includes a review of the scalp, face, mouth, hands, feet, torso and extremities, eyes and eyelids, ears, fingers, toes, and toenails. The physician makes note of any spots that need monitoring or closer examination. A skin lesion is defined as a skin area that looks different from the surrounding area. This can include an abnormal lump, bump, ulcer, sore, or colored skin area. Most lesions are harmless, but some may be skin cancer.
- Skin biopsy: If a concerning lesion is found on your skin, it will be removed and sent to a lab for examination under a microscope. This is called a skin biopsy. A biopsy is needed to diagnose BCC and SCC. The pathologist analyzes the overall appearance of the tumor and the size, shape, and type of the cells. There are several ways to do a skin biopsy. The physician chooses one based on the size and location of the affected area on the patient's body. Any biopsy is likely to leave at least a small scar. Different methods can result in various types of scars.
- During an excision biopsy, all or part of the lesion is removed. This biopsy can be done in a doctor's office or hospital. The lesion may be removed entirely during the biopsy if it is small enough.
- A skin punch biopsy removes a small piece of skin and connective tissue using a hand-held tool. Stitches are often used to close the opening in the skin.
- A skin shave biopsy can be done on the skin surface (superficial) or more profoundly. Superficial shave biopsies are helpful for very flat skin lesions.
- This type of biopsy removes the top layer of skin (epidermis) and part of the dermis using a tool similar to a razor.
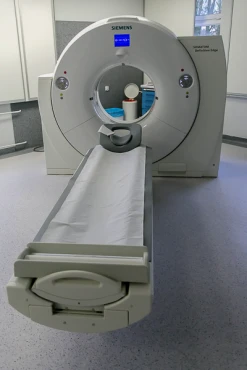
- Imaging tests such as CT scan, PET-CT scan, or MRI scan help to investigate if tumors are disseminated via metastatic process somewhere in other body parts.
- Lymph node (LN) biopsy is an option to investigate the cause of LN enlargement to confirm or exclude secondary tumor spread.
Treatment routes
What is an appropriate treatment for different BCC & SCC stages?
There are three fundamental methods to treat non-melanoma skin cancer: surgical approach, radiation therapy, and medication protocols.
Surgery is for BCC, and SCC is a radical option, meaning in the localized stage, the operation eradicates cancer. Thus, the surgical intervention is the first-line treatment. Several types of surgical operations may be applied:
- Standard surgical excision. The surgical cut removes the basal cell lesion and some normal-looking tissue surrounding it (surgical margin). Local anesthesia is used to numb the area before the surgery. Regional anesthesia is a medicine that numbs a small body area to minimize pain. The lesion is sent to pathology for further analysis.
- PDEMA/Mohs surgery. Peripheral and deep en face margin assessment (PDEMA) is a type of surgery often used to treat the head, face, hands, feet, shins, and genital areas because it can remove the cancer while sparing as much normal tissue as possible. Surgeons with special training and experience should perform it.
All forms of PDEMA allow for complete testing of the edges of any removed tissue.
Mohs surgery is the most common form of PDEMA. Mohs surgery can be done in a medical office or surgical suite and should be done by a dermatologic (skin) surgeon with special training and experience. Most patients remain awake during the procedure. After the area is numbed, the visible tumor is removed using a scalpel. Next, a thin layer of surrounding tissue is removed from under and around the wound.
The edges and underside of this tissue are evaluated by the Mohs surgeon using a microscope during the operation.
- Curettage and electrodesiccation (C&E) are done in a medical office with local numbing to the area. In this method, the visible tumor is first scraped off using a thin tool with a sharp loop or spoon at the end. Next, an electric needle is used to cauterize (burn) the base of the wound. This usually kills any remaining cancer cells and helps stop bleeding. This two-step scraping and then burning system may be done up to three times in the same session. C&E is recommended for early CSCC on the surface of the skin that has not spread to lymph nodes and for BCC patients who cannot have more invasive surgical procedures.
For regional advanced CSCC, two more surgical interventions aim to eradicate secondary lesions in the lymph nodes.
- Lymph node dissection. If lymph nodes near a squamous cell skin cancer tumor are enlarged, the doctor might biopsy them to check for cancer cells.
If the lymph node biopsy shows cancer, sometimes many nodes might be removed in a more extensive surgery called a lymph node dissection. The nodes are then looked at under a microscope for signs of cancer. This type of surgery is more comprehensive than surgery on the skin and is usually done while the patient is under general anesthesia (in a deep sleep).
- A sentinel lymph node biopsy is the first lymph node to which cancer cells most likely spread from a primary tumor. Sometimes, there is more than one sentinel lymph node.
A sentinel lymph node biopsy (SLNB) is a surgery that removes tissue samples to examine sentinel nodes. The lymph nodes are checked for cancer cells by a pathologist in a lab. Sometimes, people can have an SLNB at the same time as surgery. The results will be used to stage the cancer and plan treatment.
To locate the sentinel lymph node(s), the surgeon injects a radioactive, blue-colored substance into the patient's skin near the tumor. The substance is drained into the sentinel lymph nodes. The surgeon will identify the sentinel lymph nodes using a device and remove them through a small cut in the patient's skin. This procedure is generally done under general anesthesia.
Non-surgical physical treatment methods:
- Cryotherapy is a procedure to freeze and destroy precancerous and tumor cells using very cold liquid nitrogen. A blister and scab will form, which heals over 2 to 3 weeks.
- Photodynamic therapy (PDT) with Levulan or Photofrin – light-sensitive drugs are used to kill cancer cells using bright lamp light.
Topical therapies – treatments that are applied to the skin – include 5-fluorouracil (Carac, Efudex, Fluoroplex), imiquimod (Aldara), and tirbanibulin (Klisyri) in a prescription cream form to treat early-stage CSCC by preventing cancer cell to grow.
Systemic therapy is used in advanced forms of BCC and SCC when cisplatin/carboplatin chemotherapy, targeted anti-EGFR medications (cetuximab), and PD-1 inhibitory immunotherapy (cemiplimab and pembrolizumab) are fighting with regionally or distant metastasized SCC.
Due to the slow-growing BCC nature, radiation therapy is used only when surgical methods are unavailable. In SCC, radiotherapy aims to eradicate deep distant secondary lesions with brachytherapy or external beam radiation therapy techniques for a 3-7 weeks course that consists of 5 daily brief treatments per week.