Definition
Aortoiliac occlusive disease, or Leriche syndrome, is an occlusion of the bifurcation of the aorta and the initial parts of the common iliac arteries, which causes chronic ischemia of the pelvic organs and lower extremities. The disease is manifested by high intermittent claudication and ischemic lesions of leg tissues. In men, impotence is possible. Diagnosis of the syndrome involves ultrasound of the aorta and its branching vessels, aortography, lipid profile assessment, and coagulogram. Conservative treatment is prescribed in the early stages of the disease. Surgical methods include reconstructive aortic repair, aorto-femoral bypass, and lumbar sympathectomy.
General information
The syndrome is named after the French physiologist and surgeon René Leriche, who described the pathology in 1923. Leriche named this condition terminal aortitis and identified five main clinical manifestations. Exact data on the prevalence of abdominal aortic occlusion are unknown since some patients are asymptomatic. In European countries, the disease affects, on average, 1% of the population. Manifestation of the syndrome is typical at 40-60 years old. The ratio between men and women among patients, according to the observations of different authors, ranges from 10:1 to 30:1.
Causes
Both acquired and congenital etiologic factors can cause lesions of the terminal aorta. Pathologies that reduce the vessel’s lumen from the inside or compress the aorta from the outside contribute to the development of the syndrome. Modern angiology has established four main groups of causes that cause Leriche syndrome, which include:
- Atherosclerosis. Atheromatous plaque formation in the area of aortic bifurcation is detected in 88-94% of patients with Leriche syndrome manifestations. Atherosclerotic occlusion is characterized by slow but steady progression.
- Nonspecific aortoarteritis. Autoimmune inflammation of the aorta accounts for about 5% of the causes of Lerichesyndrome. Aortoarteritis causes occlusion symptoms predominantly in people between 20 and 40 years old.
- Thrombosis and thromboembolism. Postthromboembolic occlusion of the aortic bifurcation may result from a thrombus in the left side of the heart entering the aorta. Traumatic thrombosis caused by pelvic fractures occurs in 1% of patients.
- Rare causes. Sometimes, the development of Leriche syndrome is associated with tumors or fibrotic processes in the retroperitoneal space, compressing the aorta from the outside. Less than 1% are congenital causes, such as hypoplasia or aplasia of vessels and fibromuscular dysplasia.
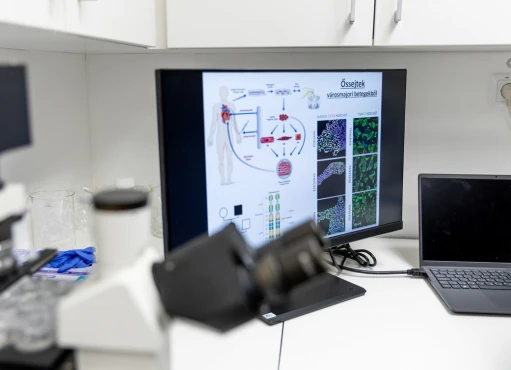
Pathogenesis
Leriche’s disease is characterized by lesions of different layers of the vascular wall, which are determined by the etiology of the process. Atherosclerosis is characterized by typical changes in the aortic intima and the formation of lipid plaques that block the vessel lumen. In aortoarteritis, the middle and outer layers of the aortic wall are predominantly thickened, and perifocal inflammation of the autoimmune type is often initiated.
The pathophysiologic basis of the disease is a progressive decrease in blood flow in the vessels of the lower extremities and pelvic organs. Due to the stealing syndrome, leading to insufficient blood flow into the inferior mesenteric artery, ischemia of the internal organs of the abdominal cavity is observed. Hemodynamically significant disorders are determined with occlusion of 60-70%. The degree of compensation of the process depends on the formation rate of vascular collaterals.
Classification
There are three types of abdominal aortic occlusion: low (distal to the inferior mesenteric artery), medium (between the inferior mesenteric artery and the renal artery), and high (at the renal artery level). More than 60% of people with Leriche syndrome have concomitant coronary or brachiocephalic artery disease.
For the choice of treatment tactics, there is a classification of aortoiliac lesions according to TASC II, according to which four types of the syndrome are distinguished:
- Type A. The patient has narrowed common iliac arteries (CIA) on one or both sides. The aorta is not involved in the pathologic process. This category also includes short (less than 3 cm) occlusions of the external iliac arteries (EIA).
- Type B represents infrarenal aortic lesions of 3 cm or less in length, bilateral CIA stenoses ranging from 3 cm to 10 cm, and EIA stenoses ranging from 3 cm to 10 cm.
- Type C. This variant of Leriche syndrome is characterized by EIA and CIA stenoses extending to 10 cm or more. In type C, occlusion spreads to the common femoral arteries (CFA).
- Type D. The most severe variant of the lesion is when the abdominal aorta and iliac arteries on both sides are involved. Multiple occlusions of the EIA and CFA are typical.
Symptoms
The first signs of Leriche syndrome are chills and paresthesias of the lower extremities. The skin of the feet and lower legs becomes very pale and cold to the touch. During walking, unpleasant pulling sensations are usually noted in the buttocks and the posterior surface of the thigh. If the process is caused by atherosclerosis, characteristic signs of this disease include xanthomas and xanthelasmas, increased fatigue, and pain behind the sternum.
The classic sign of Leriche syndrome is intermittent claudication. While walking quietly, a sharp pain in the gluteal and thigh muscles forces the person to stop. After a short rest, the pain sensations disappear. In the first degree of ischemia, patients are concerned with rapid fatigue of leg muscles. In the second degree, pain occurs when walking. In the third, pain does not disappear even at rest. The fourth degree reveals ulcerative-necrotic skin disorders.
In 20-50% of men, Leriche syndrome manifests as impotence. Lesions of the pelvic organs are also characterized by gas incontinence and difficult urination. When walking fast or climbing stairs, abdominal pain occurs, which is due to pathological redistribution of blood volume. With a prolonged course of the syndrome, the skin of the feet acquires a bluish tint, and swelling of the legs appears.
Complications
If untreated, Leriche syndrome is extremely unfavorable—5-7 years after the disease manifests, the probability of death reaches 50%. Progressive ischemia is accompanied by trophic disorders of the lower extremities. Ischemic edema increases, and ulcers form on the skin of the lower legs and feet. In the future, dry or wet gangrene of the distal parts of the leg may occur, leading to disability.
Less often, there are cardiac complications, which are due to the progression of atherosclerosis or thromboembolic processes. In Leriche syndrome, the risk of myocardial infarction and stroke increases several times. The lesion spreads to the arteries of the kidneys – death of most nephrons with the formation of terminal renal failure is observed.
Diagnosis
A preliminary diagnosis of occlusion is possible during the initial examination by a general practitioner or a vascular surgeon. Physical examination reveals the absence of pulsation of large arteries of the lower extremities. On auscultation, a systolic murmur is heard above the abdominal aorta. A decrease in the ankle-shoulder index of less than 0.7 is characteristic. To confirm Leriche syndrome, studies are carried out:
- Vascular ultrasound. Duplex scanning allows you to accurately assess the degree of narrowing of the aorta near its bifurcation to determine the features of the pathological process. Ultrasound also helps study the rate of blood flow in the femoral arteries.
- Aortography. Patients with indications for surgical treatment are subjected to an X-ray contrast study. Aortography is used to determine the exact localization and extent of the vascular lesion and assess the degree of collateral blood flow. CT of the aorta with contrast is an alternative to radiography.
- Laboratory methods. When the aortic bifurcation is occluding, analyses are referred to as auxiliary diagnostic tests. Cholesterol and lipoprotein levels are examined to confirm the occlusion syndrome’s atherosclerotic origin. A coagulogram is obligatory.
Treatment of Leriche syndrome
Conservative therapy
Drug treatment is limited to the initial degree of occlusive diseases when trophic damage to the lower limbs has not yet developed. Drugs are combined physiotherapy and dosed walking. With dyslipidemia, an appropriate diet is recommended. In Leriche’s complex, there are two main directions of therapeutic measures:
- Antiplatelet therapy. Patients are indicated a lifelong antiplatelet drug (acetylsalicylic acid) intake in low maintenance doses. Treatment is aimed at normalizing the blood coagulation system’s work and preventing thrombosis.
- Hypolipidemic therapy. Drugs that reduce cholesterol and LDL are prescribed for the atherosclerotic etiology of Leriche’s disease. Statins and fibrates are used mainly in minimal therapeutic dosages.
Surgical treatment
Surgical methods are indicated for lower limb ischemia of II-IV degree. Vascular surgeons use endovascular surgery in lesions of type A and B according to the TASC classification. For patients with type C and D syndrome, it is advisable to perform open surgical interventions on the affected vessels. Several operative techniques are used to eliminate Leriche syndrome:
- Reconstructive techniques. Resection of the altered section of the aorta with its subsequent prosthesis is considered the best way to restore blood flow in the lower part of the body. The operation is characterized by good long-term results and rarely causes thromboembolic complications.
- Aorto-femoral bypass. If blood flow in the iliac arteries is preserved, bypassing blood to the femoral arteries is indicated. The technique improves blood supply to the lower extremities by bringing arterial blood directly from the aorta.
- Lumbar sympathectomy. This operation eliminates spasms of distal vessels of the extremities in the presence of contraindications to more radical treatment methods. Sometimes, sympathectomy is performed together with revascularization to increase the effectiveness of therapy.
Prognosis and prevention
Reconstructive surgery improves the quality of life in all patients and restores the ability to work in 90% of patients. To improve the long-term results of treatment, dispensary monitoring with regular duplex scanning of vessels is recommended. Prevention of Leriche syndrome aims at timely detection and therapy of the main causes of the disease: atherosclerosis and aortoarteritis.