Comprehensive Analysis of Chronic Kidney Disease: From Diagnosis to Advanced Management Strategies
Overview
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function. The kidneys are essential for filtering waste and excess fluids from the blood, which are then excreted in urine. Advanced stages of CKD can lead to the accumulation of dangerous levels of fluid, electrolytes, and wastes in the body. Early detection and treatment are crucial in managing CKD and preventing its progression.
Risk Factors
Several factors can increase the risk of developing CKD:
- Diabetes: The leading cause of CKD, high blood sugar can damage the blood vessels in the kidneys.
- High Blood Pressure: The second leading cause, contributing to kidney damage over time.
- Heart and Blood Vessel Disease: Cardiovascular diseases can impair kidney function.
- Smoking: Smoking can interfere with the kidney's ability to filter blood and may exacerbate kidney disease.
- Obesity: Excess weight can put additional strain on the kidneys.
- Family History of Kidney Disease: A genetic predisposition to kidney issues.
- Older Age: The risk of CKD increases with age.
- Abnormal Kidney Structure: Congenital abnormalities of the kidneys can lead to CKD.
- Prolonged Use of Certain Medications: Some medications, like NSAIDs, can harm the kidneys.
Causes
CKD often stems from other medical conditions that put a strain on the kidneys:
- Diabetes (Type 1 and Type 2): Causes kidney damage over time due to high blood sugar.
- High Blood Pressure: Damages the small blood vessels in the kidneys.
- Glomerulonephritis: A group of diseases causing inflammation in the kidneys.
- Interstitial Nephritis: Inflammation of the kidney’s tubules and surrounding structures.
- Polycystic Kidney Disease: Characterized by the growth of numerous cysts in the kidneys.
- Prolonged Urinary Tract Obstruction: Can lead to kidney damage.
- Vesicoureteral Reflux: Causes urine to back up into the kidneys, potentially causing damage.
- Recurrent Kidney Infection: Can lead to lasting kidney damage.
Symptoms
Early stages of CKD often have no symptoms. As the condition progresses, symptoms may include:
- Nausea and vomiting
- Loss of appetite
- Fatigue and weakness
- Sleep problems
- Changes in urine output
- Decreased mental sharpness
- Muscle twitches and cramps
- Swelling in feet and ankles
- Persistent itching
- Chest pain and shortness of breath
- High blood pressure
Treatment
CKD treatment aims to slow the progression of kidney damage.
The treatment of CKD aims not only to slow the progression of the disease but also to address the underlying causes and manage symptoms to improve the quality of life. Here are more in-depth insights into the available treatment options:
- Blood Pressure Control
- Medications: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are commonly used to lower blood pressure and reduce strain on the kidneys.
- Lifestyle Changes: Including dietary modifications, regular exercise, and weight loss.
- Blood Sugar Management
- Medications for Diabetes: Ensuring tight control of blood sugar levels with insulin or oral hypoglycemics.
- Diet and Exercise: A diet low in sugars and carbohydrates, along with regular physical activity, helps manage diabetes effectively.
- Treating Cholesterol Levels
- Statins: These drugs are used to lower LDL ("bad") cholesterol levels, thereby reducing the risk of heart disease, a common complication of CKD.
- Anemia Management
- Iron Supplements: Oral or intravenous iron supplements to address iron-deficiency anemia.
- Erythropoiesis-Stimulating Agents (ESAs): Medications that stimulate the bone marrow to produce more red blood cells.
- Mineral and Bone Disorder Treatment
- Phosphate Binders: Prevent high phosphate levels by binding phosphate in the gut.
- Vitamin D Supplements: To correct vitamin D deficiency, which is common in CKD.
- Calcimimetics: Medications that lower parathyroid hormone levels, which can be elevated in CKD.
- Dietary Adjustments
- Nutritionist Consultation: Working with a dietitian to develop a kidney-friendly eating plan.
- Reduced Protein Intake: To decrease the buildup of waste products in the blood.
- Limiting Fluids: Managing fluid intake to prevent fluid overload, especially in later stages of CKD.
- Dialysis
- Hemodialysis: A machine filters waste and excess fluids from the blood, typically done several times a week at a dialysis center.
- Peritoneal Dialysis: Involves surgically placing a catheter into the abdomen and using the lining of the abdomen to filter the blood inside the body.
- Kidney Transplantation
- Donor Kidney: Receiving a kidney from a living or deceased donor.
- Immunosuppressive Therapy: Medications to prevent the body from rejecting the new kidney.
- Managing Complications
- Cardiovascular Treatments: Addressing any heart-related complications.
- Electrolyte Imbalance Management: Regular monitoring and adjustments in medication or diet to maintain electrolyte balance.
- Lifestyle Modifications
- Smoking Cessation: Essential for overall kidney health.
- Exercise: Regular physical activity tailored to the individual's capacity.
- Stress Management: Techniques like meditation or counseling to manage stress.
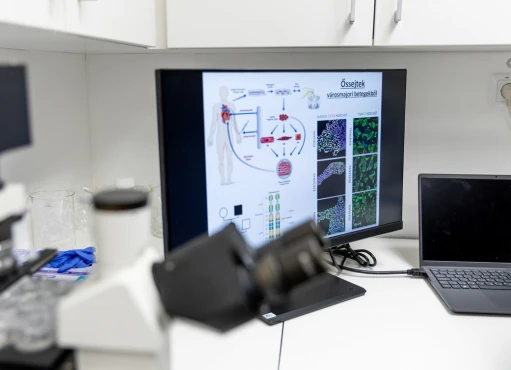
Experimental and Emerging Therapies
- Stem Cell Research: Exploring the potential of stem cells in repairing damaged kidney tissue.
- Gene Therapy: Investigating genetic factors and potential genetic treatments.
- New Pharmacological Agents: Development of novel drugs targeting specific pathways involved in CKD progression.
Holistic and Supportive Care
- Psychological Support: Addressing the mental health challenges associated with living with a chronic illness.
- Palliative Care: For advanced CKD, focusing on quality of life and symptom control.
Complications
CKD can lead to numerous complications, affecting various parts of the body:
- Fluid retention, leading to swelling and hypertension.
- Sudden changes in potassium levels, potentially affecting heart function.
- Cardiovascular diseases.
- Weak bones and increased risk of fractures.
- Anemia and decreased sex drive.
- Central nervous system damage.
- Decreased immune response.
- Pericarditis, an inflammation of the heart's outer lining.
- Complications in pregnancy.
- End-stage kidney disease, necessitating dialysis or transplantation.
Prevention
- Preventive measures can reduce the risk of developing CKD:
- Follow Instructions for OTC Medications: Especially those that can harm the kidneys.
- Maintain a Healthy Weight: To ease the strain on kidneys.
- Quit Smoking: Smoking can exacerbate kidney damage.
- Manage Existing Health Conditions: Keeping diabetes, hypertension, and other conditions under control.
- Stay Hydrated: Adequate hydration helps the kidneys function properly.
- Eat a Balanced Diet: Low in sodium and processed meats.
- Regular Exercise: Helps in maintaining overall health.
Conclusion
Chronic Kidney Disease is a serious health condition, but with early detection and proper management, its progression can be slowed, and quality of life can be maintained. Understanding the risk factors, causes, and symptoms of CKD is essential for those at risk or already diagnosed with the condition. Through a combination of lifestyle changes, medication, and regular medical check-ups, individuals with CKD can manage their condition effectively.