Introduction
Amyloidosis is a general, systemic disease of the body in which a specific glycoprotein (amyloid) is deposited in organs and tissues with impaired function of the latter. Amyloidosis can affect the kidneys (nephrotic syndrome, edema syndrome), heart (heart failure, arrhythmias), GI tract, musculoskeletal system, and skin. The development of polyserositis, hemorrhagic syndrome, and psychiatric disorders is possible. Reliable diagnosis of amyloidosis is facilitated by detecting amyloid in biopsy samples of affected tissues. To treat amyloidosis, immunosuppressive and symptomatic therapy is given; peritoneal dialysis and kidney and liver transplantation are also indicated.
General information
Amyloidosis is a disease from the group of systemic dysproteinoses, which proceeds with the formation and accumulation of a complex protein-polysaccharide compound – amyloid – in tissues. The prevalence of amyloidosis in the world is primarily geographically determined: for example, periodic disease is more common in the countries of the Mediterranean basin; amyloid polyneuropathy – in Japan, Italy, Sweden, Portugal, etc. The average incidence of amyloidosis in the population is 1 case per 50,000. The disease usually develops in persons older than 50-60 years. Since amyloidosis affects almost all organ systems, the disease is studied by various medical disciplines: rheumatology, urology, cardiology, gastroenterology, neurology, and others.
Causes of amyloidosis
The etiology of primary amyloidosis has yet to be fully understood. At the same time, it is known that secondary amyloidosis is usually associated with chronic infectious (tuberculosis, syphilis, actinomycosis) and purulent-inflammatory diseases (osteomyelitis, bronchiectasis, bacterial endocarditis, etc.), less often – tumor processes (lymphogranulomatosis, leukemia, cancer of visceral organs). Reactive amyloidosis can develop in patients with atherosclerosis, psoriasis, rheumatologic diseases (rheumatoid arthritis, Bechterew’s disease), chronic inflammation (nonspecific ulcerative colitis, Crohn’s disease), multisystemic lesions (Whipple’s disease, sarcoidosis). Among the factors contributing to the development of amyloidosis, hyperglobulinemia, dysfunction of cellular immunity, genetic predisposition, etc., are of primary importance.
Pathogenesis
Among the numerous theories, the theory of dysproteinosis, local cellular genesis, and immunologic and mutational theories have the most supporters. The theory of local cellular genesis considers only the processes occurring at the cellular level (formation of fibrillar amyloid precursors by the macrophage system), while the formation and accumulation of amyloid occurs outside the cell. Therefore, the theory of local cellular genesis must be considered only partially.
According to the theory of dysproteinosis, amyloid is a product of abnormal protein metabolism. The main links in the pathogenesis of amyloidosis – dysproteinemia and hyperfibrinogenemia contribute to the accumulation of coarsely dispersed fractions of protein and paraproteins in the plasma.
Amyloid is a complex glycoprotein consisting of fibrillar and globular proteins closely associated with polysaccharides. Amyloid deposits accumulate in the intima and adventitia of blood vessels, stroma of parenchymatous organs, glandular structures, etc. A pronounced accumulation of amyloid is accompanied by macroscopic changes in the affected organ (volume increase, greasy or waxy appearance). Amyloidosis results in stromal sclerosis and atrophy of organ parenchyma, their clinically significant functional failure.
Classification
According to the causes, primary (idiopathic), secondary (reactive, acquired), hereditary (familial, genetic), and senile amyloidosis are distinguished. Various forms of hereditary amyloidosis occur in Mediterranean fever, or periodic disease (fever attacks, abdominal pain, constipation, diarrhea, pleurisy, arthritis, skin rashes), Portuguese neuropathic amyloidosis (peripheral polyneuropathy, impotence, cardiac conduction disorders), Finnish type (corneal atrophy, cranial neuropathy), Danish variant (cardiopathic amyloidosis), etc.
Depending on the predominant involvement of organs and systems, nephropathic (renal amyloidosis), cardiopathic (cardiac amyloidosis), neuropathic (amyloidosis of the nervous system), hepatopathic (liver amyloidosis), epinephropathic(adrenal amyloidosis), skin amyloidosis and mixed type of the disease are distinguished. In addition, it is customary to distinguish between localized and generalized (systemic) amyloidosis in international practice. Localized forms, usually developing in older adults, include amyloidosis in Alzheimer’s disease, type 2 diabetes mellitus, endocrine tumors, skin tumors, bladder tumors, and others. Depending on the biochemical composition of amyloid fibrils, the following types are distinguished among systemic forms of amyloidosis:
- AL – light chains of Ig in the fibrils (in Waldenström’s disease, myeloma disease, malignant lymphomas);
- AA – as part of fibrils acute-phase serum α-globulin, similar in its characteristics to C-reactive protein (in tumor and rheumatic diseases, periodic disease, etc.);
- Aβ2M- within β2-microglobulin fibrils (in chronic renal failure in patients on hemodialysis);
- ATTR – as part of the fibrils transport protein transthyretin (in familial hereditary and senile forms of amyloidosis).
Symptoms of amyloidosis
Clinical manifestations of amyloidosis are diverse and depend on the severity and localization of amyloid deposits, the biochemical composition of amyloid, the “seniority” of the disease, and the degree of organ dysfunction. In the latent stage of amyloidosis, when amyloid deposits can be detected microscopically, there is no symptomatology. With the development and progression of functional insufficiency of one or another organ, clinical signs of the disease increase.
In renal amyloidosis, a long-lasting stage of moderate proteinuria is replaced by the development of nephrotic syndrome. Transition to the advanced stage may be associated with intercurrent infection, vaccination, hypothermia, and exacerbation of the underlying disease. Edema gradually increases (first on the legs and then on the whole body), and nephrogenic arterial hypertension and renal failure develop. Thrombosis of renal veins may occur. Massive protein loss is accompanied by hypoproteinemia, hyperfibrinogenemia, hyperlipidemia, and azotemia. The urine reveals micro-, sometimes macrohematuria and leukocyturia. In general, renal amyloidosis is characterized by an early edema-free stage, edematous stage, and uremic (cachectic) stage.
Cardiac amyloidosis proceeds as restrictive cardiomyopathy with typical clinical signs—cardiomegaly, arrhythmia, and progressive heart failure. Patients complain of dyspnea, edema, and weakness occurring with minor physical exertion. Less often, polyserositis (ascites, exudative pleuritis, and pericarditis) develops in cardiac amyloidosis.
Gastrointestinal damage in amyloidosis is characterized by amyloid infiltration of the tongue (macroglossia), esophagus (rigidity and impaired peristalsis), stomach (heartburn, nausea), and intestine (constipation, diarrhea, malabsorption syndrome, intestinal obstruction). Gastrointestinal bleeding at various levels may occur. With amyloid infiltration of the liver, hepatomegaly, cholestasis, and portal hypertension develop. Pancreatic damage in amyloidosis is usually masked by chronic pancreatitis.
Amyloidosis of the skin occurs with multiple waxy plaques (papules, nodules) in the face, neck, and natural skin folds. External signs indicate that the skin lesion may resemble scleroderma, neurodermatitis, or red squamous lichen planus. Myopathy is typical for amyloid lesions of the musculoskeletal system, the development of symmetric polyarthritis, carpal tunnel syndrome, and brachial periarthritis. Some forms of amyloidosis with involvement of the nervous system may be accompanied by polyneuropathy, paralysis of the lower extremities, headaches, dizziness, orthostatic hypotension, sweating, dementia, etc.
Diagnosis
Various clinicians, including rheumatologists, urologists, cardiologists, gastroenterologists, neurologists, dermatologists, therapists, and others, can encounter clinical manifestations of amyloidosis. Of primary importance for the correct diagnosis is a comprehensive assessment of clinical and anamnestic signs and a comprehensive laboratory and instrumental examination.
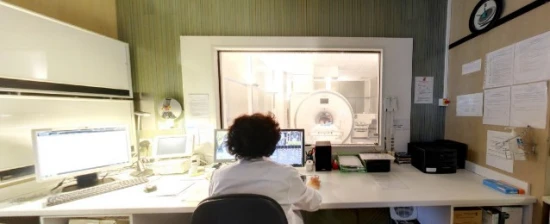
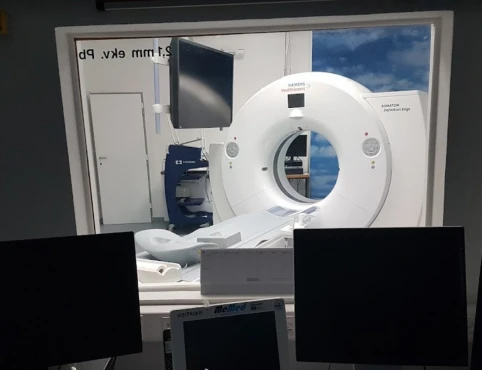
Echocardiography and ECG are appointed to assess the functional state of the cardiovascular system. Examination of the digestive tract involves ultrasound of the abdominal cavity, radiological tests (esophagus, stomach X-ray), and endoscopic studies (EGD, sigmoidoscopy). Amyloidosis should be thought of when the combination of proteinuria, leukocyturia, with hypoproteinemia, hyperlipidemia (increase in blood cholesterol, lipoproteins, triglycerides), hyponatremia and hypocalcemia, anemia, decreased platelet count. Electrophoresis of blood serum and urine allows to determine the presence of paraproteins.
Detecting amyloid fibrils in the affected tissues makes the final diagnosis of amyloidosis possible. For this purpose, a kidney, lymph nodes, gums, gastric mucosa, and rectum biopsy may be performed. A thorough medical and genetic analysis of the pedigree facilitates establishing the hereditary nature of amyloidosis.
Treatment of amyloidosis
The lack of completeness of knowledge about the etiology and pathogenesis of the disease causes the difficulties associated with the treatment of amyloidosis. In secondary amyloidosis, active therapy of the background disease is important. Dietary recommendations suggest limiting the intake of table salt and protein and the inclusion of raw liver in the diet. Symptomatic therapy of amyloidosis depends on the presence and severity of specific clinical manifestations as pathogenetic therapy may be prescribed drugs of 4-aminoquinoline series (chloroquine), dimethyl sulfoxide, unitiol, and colchicine. Treatment regimens with cytostatics and hormones (melfolan+prednisolone, vincristine+doxorubicin+dexamethasone) treat primary amyloidosis. In the development of CKD, hemodialysis or peritoneal dialysis is indicated. In some cases, the question of kidney or liver transplantation is raised.
Prognosis
The course of amyloidosis is progressive, almost irreversible. The disease can be aggravated by amyloid ulcers of the esophagus and stomach, bleeding, hepatic failure, diabetes mellitus, and others. If chronic renal failure develops, the average life expectancy of patients is about one year; if heart failure develops, it is about four months. The possibility of therapy for the underlying disease determines the prognosis of secondary amyloidosis. A more severe course of amyloidosis is noted in elderly patients.