Disease Types
What is the acoustic neuroma?
Acoustic neuroma, or vestibular schwannoma, is a non-cancerous growth that develops on the eighth cranial nerve, which controls balance and hearing. While these tumors are benign, they can still cause significant health problems due to their location near vital brain structures. Acoustic neuromas account for approximately 8-10% of all intracranial tumors, with an incidence rate of around 1 to 2 cases per 100,000 people annually. Most cases are diagnosed in individuals between 30 and 60, with no significant gender differences. Most acoustic neuromas occur spontaneously, but about 5% are associated with neurofibromatosis type 2, a genetic disorder [Kim et al., 2023].
Acoustic neuromas are classified based on their size and location. Untreated, these tumors typically grow slowly, with some remaining stable for years. However, they can compress nearby nerves, blood vessels, and brain structures as they expand, leading to various symptoms.
- Small acoustic neuroma (Intracanalicular, <2 cm) tumors are confined to the internal auditory canal or starting to grow into the cerebellopontine angle. Patients may experience hearing loss, ear ringing (tinnitus), and mild balance issues.
- Medium-sized tumors (Cerebellopontine Angle, 2-4 cm) extend further into the cerebellopontine angle and can start compressing the brainstem. Symptoms often include more pronounced hearing loss, worsening balance problems, and facial numbness.
- Large acoustic neuromas (>4 cm) significantly compress the brainstem and surrounding structures. This can lead to severe balance problems, difficulty swallowing, headaches, and the buildup of fluid in the brain (hydrocephalus).
Causes & Risk Factors
What is the primary issue of acoustic neuroma?
The exact cause of acoustic neuroma is often linked to a malfunction in the NF2 gene on chromosome 22. This gene normally produces a protein that suppresses tumor growth, but tumors can develop along the vestibulocochlear nerve in its absence. Some key risk factors include:
- Genetics: neurofibromatosis type 2 is a hereditary condition that significantly increases the chances of developing acoustic neuromas on both sides of the head.
- Radiation exposure: prior exposure to the head or neck, especially during childhood, may raise the risk.
- Age: most cases are diagnosed in individuals between 30 and 60 years old.
- Environmental factors: although not well-established, prolonged exposure to loud noises has been suggested as a potential risk factor.
Clinical Manifestation & Symptoms
What signs should one anticipate while suspecting acoustic neuroma?
The symptoms of acoustic neuroma are typically related to the tumor's impact on hearing and balance. Hearing loss is the most common symptom, often occurring gradually in one ear, though it can also develop suddenly. Patients may also experience tinnitus, a ringing or buzzing sound in the affected ear. As the tumor affects the vestibular portion of the nerve, individuals may struggle with dizziness and balance issues. In cases where the lesion is large, it may compress the facial nerve, leading to numbness, tingling, or weakness in the face. Additionally, large tumors can cause headaches and vision changes due to increased pressure within the skull.
These symptoms can significantly impact a person's quality of life, making it crucial to seek medical attention if any of these signs are present. Early detection and appropriate treatment can help manage the condition and prevent further complications [NHS UK, 2024].
Diagnostic Route
When, where, and how should acoustic neuroma be detected?
The diagnostic evaluation of acoustic neuroma typically begins with a thorough clinical examination, focusing on hearing, balance, and neurological function. There are the following diagnostic tools:
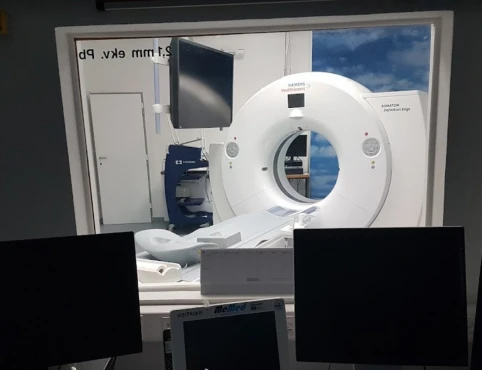
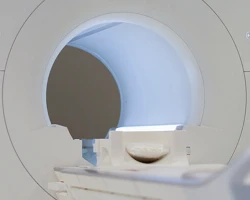
- Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing acoustic neuroma. MRI with gadolinium contrast can detect even small tumors confined to the internal auditory canal.
- Audiometry is a hearing test used to evaluate the degree of hearing loss, which is often the first symptom.
- Vestibular Testing assesses balance function, which can be affected by the tumor.
- Brainstem Auditory Evoked Potentials (BAEP) measure the electrical activity in the brainstem in response to sound, which helps evaluate the function of the auditory pathway.
Treatment Approaches
What are the options for managing acoustic neuroma?
Watchful Waiting (Observation)
Watchful waiting may be the most suitable approach for certain patients with acoustic neuroma. This option is particularly appropriate for older individuals, those with small tumors that are causing minimal symptoms, or patients who have significant health issues that could make surgery or radiation therapy too risky.
Under this approach, healthcare providers closely monitor the patient's condition through regular MRI scans and hearing evaluations. They help closely monitor the tumor, watching for any significant growth or worsening symptoms. If the tumor expands rapidly or the patient's symptoms worsen, the medical team may reconsider active treatment options.
Interestingly, around 30-50% of observed acoustic neuromas show little to no growth over several years, making watchful waiting a viable choice for some patients. However, it's important to note that even with this conservative approach, there remains a risk of progressive hearing loss over time. Watchful waiting can be a reasonable management strategy for carefully selected patients, providing a balanced approach that avoids unnecessary interventions while closely monitoring the condition.
Microsurgical Resection
Microsurgical resection is recommended for young, healthy patients with large tumors or those causing significant brainstem compression. There are several surgical approaches to consider.
The retrosigmoid approach provides access to the cerebellopontine angle and aims to preserve hearing in patients with small tumors. The translabyrinthine approach is used for larger tumors or when hearing preservation is not possible. This approach involves removing the bone behind the ear, leading to hearing loss but offering excellent access to the tumor. The middle fossa approach is suitable for small tumors confined to the internal auditory canal, intending to preserve hearing.
The efficacy of microsurgical resection is high, with tumor control rates exceeding 90%. However, the risk of complications, such as facial nerve damage and hearing loss, can be significant. Fortunately, advances in intraoperative monitoring of cranial nerves have significantly improved outcomes, reducing the risk of nerve damage and improving the overall prognosis for patients undergoing this treatment option.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery is a suitable treatment option for patients with small to medium-sized acoustic neuromas, as well as for elderly individuals or those who may not be able to undergo surgery. This non-invasive procedure offers two main methods:
The Gamma Knife approach delivers a single, precise high-dose radiation treatment, while the CyberKnife allows for a fractionated treatment plan, which may help reduce the risk of side effects. Both techniques have demonstrated impressive tumor control rates, typically 85% to 95%, and carry a relatively low risk of facial nerve damage. Regarding hearing preservation, 50% to 70% of SRS patients can retain adequate hearing.
An exciting advantage of stereotactic radiosurgery is that it is typically performed on an outpatient basis, enabling patients to resume their normal activities after the procedure quickly. This non-invasive approach makes it a convenient and accessible treatment option for many individuals diagnosed with acoustic neuroma.
Prognosis & Follow-up
How does cutting-edge science improve the lifespan and quality of life for those with acoustic neuroma?
Acoustic neuromas can lead to significant complications without treatment due to their progressive nature. As the tumor grows, it can cause irreversible hearing loss, persistent balance problems, facial nerve paralysis, and life-threatening brainstem compression. The severity of these complications increases with tumor size and location, emphasizing the importance of timely diagnosis and treatment.
<br/>Patients who do not receive treatment for acoustic neuroma may experience worsening symptoms, such as profound hearing loss, severe vertigo, facial nerve damage, and neurological deficits. In extreme cases, large untreated tumors can increase intracranial pressure, cause hydrocephalus, and potentially lead to fatal brainstem compression.
<br/>The prognosis for patients who receive treatment for acoustic neuroma depends on the tumor size at diagnosis, the chosen treatment approach, and the patient's overall health. Long-term survival is excellent, with a nearly 100% survival rate for benign tumors. However, complications like hearing loss, balance issues, and facial nerve dysfunction can still impact the patient's quality of life.
Ongoing follow-up is essential to check for any tumor recurrence or growth, especially for patients who opt for watchful waiting or incomplete tumor removal. Typical follow-up includes:
- MRI scans every 6-12 months for the first few years, then annually if the tumor remains stable.
- Regular hearing tests to assess auditory function.
- Neurological assessments to monitor for any new or worsening symptoms, particularly in facial nerve function.
Patients treated with radiosurgery require lifelong monitoring, as there is a slight chance of delayed tumor growth even years after the procedure. Monitoring for radiation-related changes is also necessary.