What’s that?
Acute ischemia of a limb (leg or arm) is a severe vascular disease threatening the loss of a limb, i.e., amputation of a leg or arm. Lack of oxygen in the leg tissues occurs due to impaired blood flow in the arteries.
Pathologies of the central and peripheral arteries of the lower extremities account for 18% of all cardiovascular diseases. They occur in about 3-4% of the population and in older people – in 5-10% of the population.
Reasons
Acute ischemia is a complication of chronic heart and vascular disease. It always occurs suddenly, without precursors. Acute ischemia results from rapid occlusion of a large limb artery by detached thrombus fragments from the aorta or heart (embolism). Another cause is atherothrombosis. Closure of a major artery can lead to fatal disruption of blood supply to the arm or leg.
The most common causes of ischemia are diseases of the arteries of the legs, such as:
- atherosclerosis;
- endarteritis and thromboangiitis (inflammatory diseases of the arteries);
- thrombosis;
- trauma to the arterial wall.
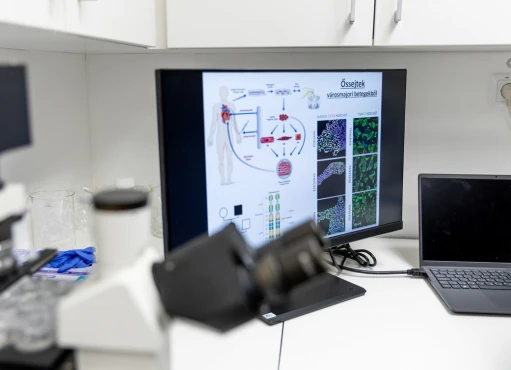
In more than 97% of cases, the leading cause of leg ischemia is atherosclerosis of the arteries of the lower extremities. This disease develops due to inflammation and disruption of the endothelium – the cells of the inner layer of the arteries. The appearance of atherosclerotic plaques accompanies it and leads to changes in blood movement through the vessels.
Symptoms
Symptoms of leg ischemia depend on the severity of the condition.
Critical limb ischemia
Due to the significant lesion, the perfusion pressure in the leg is critically reduced, and compensatory mechanisms cannot prevent tissue oxygen deficiency. It leads to pain syndrome. It is represented by pronounced pain at rest, which is poorly relieved by narcotic analgesics, especially at night.
Against the background of this condition, ulcers appear on the nail phalanges of the fingers, in the heel area, and between the toes. They may be infected and accompanied by cellulitis and inflammation of the lymph nodes.
The ulcers have jagged edges. Their bottom is covered with a fibrinous plaque. Such gangrenous changes more often affect the fingertips and, in the absence of infection, can lead to mummification and rarely to spontaneous amputation. As a result, in the natural course, inadequate treatment or lack thereof, critical ischemia leads to loss of the limb.
Acute limb ischemia
This condition is characterized by a sharp decrease in blood supply to the limb, threatening its viability. It occurs suddenly against the background of an imaginary “complete well-being,” often leading to gangrene.
The leading causes of critical ischemia:
- atherothrombosis – 41% of cases;
- embolism – 36% of cases;
- thrombosis of prostheses and endovascular intervention zones (surgery on vessels without incisions) – up to 16% of cases.
The first signs of acute ischemia are pain in the affected limb, numbness, coldness, and paresthesias. The skin becomes pale, later supplemented by a bluish tint. Skin temperature is sharply reduced, especially in the foot and lower leg area. There are pronounced sensory disorders, decreased muscle strength in the affected limb (paresis), or the person completely loses the ability to move (paralysis).
Pain on palpation of the calf muscles is an unfavorable sign characteristic of subfascial edema, a sign of severe ischemia.
Further development of muscle contracture indicates irreversible dying of the limb and is a precursor to gangrene.
Diagnosis of lower limb ischemia
Diagnosis requires clarification of the medical history and analysis of complaints, examination, physical examination, and instrumental diagnosis.
Initial diagnosis
The following factors will indicate the presence of arterial disease in the legs:
- complaint and history analysis data:
- walking impairment;
- pain at rest;
- presence of lesions in other arterial basins.
- physical exam findings:
- pulsation changes seen on palpation;
- a non-healing ulcer on his leg;
- gangrene of the fingers;
- pallor, change in skin temperature, lack of hair, and poor muscular development.
Instrumental diagnostics
Ankle-brachial index measurement is a non-invasive method of examining the arteries of the extremities. Its essence is to measure the systolic blood pressure in the brachial arteries and arteries of the foot after lying on a couch for 10 minutes. This test is reliable and can be used as a first-line method.
An index ≤ 0.9 indicates lower extremity disease. High values indicate increased arterial tone, characteristic of patients with diabetes mellitus and/or chronic kidney disease. With borderline values, a stress test is required. Ultrasound duplex scanning
Vascular ultrasound is the first-line diagnostic method. It allows to assess the anatomy of the lesion, blood flow through the vessels and morphology, and verify the treatment results. Measurement of the degree of stenosis and criteria for qualitative and quantitative analysis of the blood flow spectrum are used to determine the nature of the lesion**.**
CT angiography is necessary to clarify the lesion’s anatomy and plan surgery. For this purpose, a contrast agent is injected intravenously. The image is modeled from a series of cross-sectional scans.
Treatment
The sooner the operation to restore the blood supply is performed, the higher the probability of preserving the affected limb and restoring sensation and motor functions completely!
The main factor in successful treatment is time. Performing surgery within hours of the onset of symptoms can save the limb in 100% of cases. If a day has passed and paralysis has developed, treatment results are not so optimistic. If more than a day has passed, saving the limb is only sometimes possible. In this case, the question arises about the level of amputation.
Endovascular procedures – repairing blood vessels without incisions:
- Thrombectomy – mechanical removal of the thrombus that caused the artery blockage using a Fogarty catheter. Blood flow in the limb is restored.
- Transluminal balloon angioplasty – insertion of a thin tube with a tiny balloon into the artery to widen the vessel;
- stenting – placement of a resilient metal frame in the vessel lumen to widen the lumen of the artery.
Open surgeries:
- Bypassing with synthetic vascular and/or autovenous grafts – creating an additional bypass pathway of blood supply;
- open and/or closed endarterectomy – removal of atherosclerotic plaques;
- vessel repair with vascular patches.
Hybrid surgeries are performed for multistage and combined arterial lesions, combining X-ray and conventional surgery techniques.
Prevention
Risk factors for the development of acute limb ischemia are hereditary predisposition, smoking, atherosclerosis, heart rhythm disorders (arrhythmia), and arterial hypertension. Regularly visit your family doctor and follow his recommendations. It is essential to detect diseases of the heart and blood vessels promptly. Arrhythmia is one of the leading causes of blood clots. It can be hidden without symptoms; its detection is essential for doctors of different specialties.