Myocardial infarction - etiology, pathogenesis
Acute myocardial infarction (MI) is one of the most common diagnoses in hospitalized patients in industrialized countries. MI occurs as a result of an acute lack of oxygen due to a violation of its delivery to the heart muscle (myocardium), resulting in the death of heart tissue. This process is characterized by certain causes and mechanisms, the understanding of which is important for maintaining health.
What is the difference between ST-elevation and non-ST-elevation MI?
The ST segment is a specific area on a patient's ECG. Identification of its rise is very important for further management of the patient. Incomplete restriction of blood flow to the site of the heart characterizes unstable angina, which can lead to non-ST elevation myocardial infarction (NSTEMI). Complete and sudden occlusion (narrowing) of a coronary artery is usually associated with ST-segment elevation myocardial infarction (STEMI).
What is the difference between unstable angina and NSTEMI?
In NSTEMI, due to damage and destruction of heart cells, the level of troponins (molecules that are released from the heart muscle when it is damaged) in the blood is increased, while in unstable angina, the concentration of these markers is normal.
What is acute coronary syndrome (ACS) and how is it related to myocardial infarction?
Symptoms of MI of different types are also similar to those of angina pectoris. Without a blood test and an ECG, it will be difficult for the medical team to make an accurate diagnosis, therefore, until a specific pathology (for example, ST-segment elevation myocardial infarction) is identified, the patient's condition is referred to as acute coronary syndrome.
What is the cause (etiology) of MI?
Depending on the cause of MI, 5 types of this pathology are distinguished:
- MI as a result of rupture or erosion of atherosclerotic plaques; with the formation of a blood clot or hemorrhage into the plaque.
- MI due to a mismatch between oxygen supply and demand for it; without the destruction of plaques and the formation of blood clots (for example, with severe anemia or respiratory failure).
- Sudden unexpected cardiac death that occurs before troponin levels can be measured. In this type, a person has recent changes in the ECG or MI is detected at autopsy.
- Heart attack associated with percutaneous coronary intervention (subtype 4a), stent thrombosis (subtype 4b), or restenosis (recurrent blockage) in a coronary artery where a stent was previously placed.
- MI associated with coronary artery bypass surgery.
ACS develops most often as a result of the formation of a thrombus on a damaged atherosclerotic plaque (type I myocardial infarction), which reduces the patency of the coronary artery and, accordingly, disrupts blood flow. This leads to an imbalance between the heart muscle's oxygen demand and oxygen supply. Ischemia and damage to cardiomyocytes occur.
The following factors also increase the risk of developing myocardial infarction:
- diabetes;
- smoking;
- hypertension;
- high level of cholesterol;
- hyperlipidemia;
- passive lifestyle;
- diet high in fat;
- stress;
- metabolic syndrome;
- family history of ischemic heart disease (including MI and sudden cardiac death);
- the presence of first-degree relatives who underwent coronary revascularization;
- age;
- belonging to the male sex;
- obesity.
Thus, some patients with MI may have a large number of risk factors at the same time. Less common conditions that predispose people to a heart attack are:
- hypercoagulability (a change that leads to increased thrombus formation);
- disease of collagen vessels;
- abuse of cocaine;
- intracardiac thrombi or masses that can cause blockage of the coronary arteries.
Can acute myocardial infarction occur after chest and heart injury?
Myocardial infarction is an uncommon complication in patients with chest trauma. Due to the latter, damage to the vessels of the heart can occur. This leads to MI due to coronary spasm, thrombosis, rupture or dissection of the arterial wall. Patients with underlying coronary artery disease are more susceptible to ACS in trauma as a result of limited coronary reserve, excess circulating catecholamines (eg, adrenaline), hypoxia (oxygen starvation), blood loss, and decreased blood pressure.
More commonly, the patient may experience cardiogenic syncope (fainting) due to an arrhythmia due to trauma, which also often leads to an increase in the level of markers specific for MI (troponin) without significant coronary artery stenosis. This requires the doctor to correctly interpret laboratory tests in such a patient.
Is pregnancy a risk factor for MI?
As the age of the pregnant woman increases, the risk of acute myocardial infarction increases (especially for women older than 45-50 years). In addition to other factors, pregnancy increases the risk of a heart attack by 3 to 4 times. The frequency of MI during pregnancy ranges from 3 to 100 per 100,000 births. Maternal mortality reaches 11%, and the associated fetal mortality is 9%.
Pathogenesis of myocardial infarction with ST segment elevation
This type of MI usually occurs with a sharp decrease in coronary blood flow after thrombotic occlusion of a coronary artery previously affected by atherosclerosis. Slowly developing stenosis (narrowing) of the coronary arteries of a high degree usually does not provoke ST-segment elevation MI. This is due to the fact that over time, a collateral network of vessels is formed that feeds the heart.
A STEMI occurs when a blood clot in a coronary artery develops rapidly at the site of an injury to the vessel. In most cases, with the destruction of an atherosclerotic plaque and the appearance of conditions (local or systemic) that promote thrombosis, a parietal thrombus forms at the site of plaque rupture and the affected coronary artery becomes blocked.
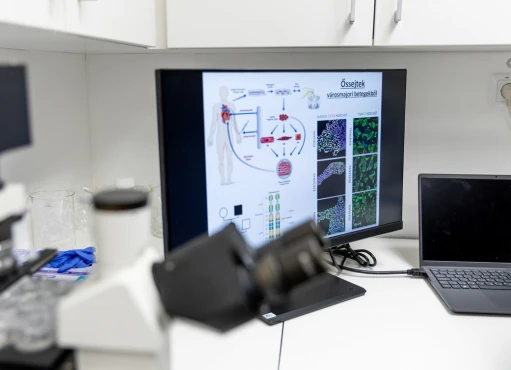
Histological studies (studies of heart tissue) show that coronary plaques, prone to destruction, have a rich lipid core and a thin fibrous membrane. After the initial layer of platelets is formed at the site of the destroyed plaque, various triggers (collagen, ADP, adrenaline, serotonin) contribute to their activation.
After stimulation of platelets, thromboxane A2 is released, a strong local vasoconstrictor (vasoconstrictor) agent, further activation of platelets occurs and potential resistance to fibrinolysis (destruction of a blood clot) develops.
In addition to the formation of thromboxane A2, platelet activation promotes changes in glycoprotein IIb/IIIa receptors, which are converted and develop a high affinity for soluble adhesive (binding) proteins such as fibrinogen. The latter can simultaneously bind to two different platelets, which leads to compaction and platelet aggregation.
Also, with the development of MI, the so-called coagulation cascade is formed. It is activated after damage to arterial cells at the site of plaque rupture. As a result of this cascade, the coronary vessel is eventually blocked by a thrombus containing platelet aggregates and fibrin strands.
In rare cases, STEMI may be precipitated by coronary artery occlusion caused by coronary embolism, congenital anomalies, coronary spasm, or a wide range of systemic, especially inflammatory, diseases.
Pathogenesis of STEMI
NSTEMI is most commonly caused by an imbalance between oxygen supply and demand, which results from partial occlusion of a vessel by a thrombus. This thrombus is formed on the destroyed atherosclerotic coronary plaque or due to erosion of the endothelium of the coronary arteries.
Other causes of non-ST elevation myocardial infarction include:
- Severe mechanical obstruction (blockage of the vessel) due to progressive coronary atherosclerosis.
- Dynamic obstruction (for example, coronary spasm, as in Prinzmetal's variant angina).
- Increased myocardial oxygen demand (for example, with an increase in heart rate, provoked by an increase in body temperature).
More than one of these processes may be involved.
Statistically, in NSTEMI, approximately 10% of patients have left main coronary artery stenosis, 35% have three-vessel disease, 20% have two-vessel disease, 20% have single-vessel occlusion, and 15% have no overt coronary artery stenosis.
Patients with NSTEMI often have several atherosclerotic plaques that are at risk of destruction (so-called vulnerable plaques).
What determines the degree of damage to the heart muscle?
The amount of myocardial damage caused by coronary occlusion depends on:
- the volume of tissue supplied by the affected vessel;
- the degree of blockage of the vessel (full or partial occlusion) and its duration;
- the volume of blood supplied through the collateral vessels to the affected tissue;
- myocardial oxygen demand;
- internal (endogenous) factors that can cause early spontaneous lysis (destruction) of an occlusive thrombus;
- the adequacy of myocardial blood supply in the infarction zone when blood flow is restored.
Thus, myocardial infarction can have a different etiology. The disease is characterized by risks that are similar to those of other diseases of the heart and blood vessels (for example, smoking or obesity). Incomplete restriction of blood flow to the heart can lead to non-ST elevation myocardial infarction (NSTEMI). Complete and sudden occlusion of a coronary artery is usually associated with ST-segment elevation myocardial infarction (STEMI).
References:
- Glenn N. Levine. Cardiology Secrets, 5th Edition. 2018. ISBN-13: 978-0323478700.
- Netter’s cardiology, third edition. 2019. ISBN: 978-0-323-54726-0.
- Harrison`s Principles of Internal Medicine 19/E (Vol.1). Dennis Kasper, Anthony Fauci, Stephen Hauseret all. McGraw-HillEducation 2015 ISBN: 0071802134 ISBN-13(EAN): 9780071802130.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177.
- 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2021;42(23):2298.