Thoracic aortic aneurysm (TAA) - disease classification, clinical presentation and diagnosis
An aneurysm is a pathologically enlarged section of an artery. The disease occurs in the form of both congenital and acquired pathology. Aneurysms can occur in any artery. In this article, we will analyze the classification, clinical picture and diagnosis of one of the most common forms of this pathology - thoracic aortic aneurysm. We will also answer the question of who is most susceptible to this disease.
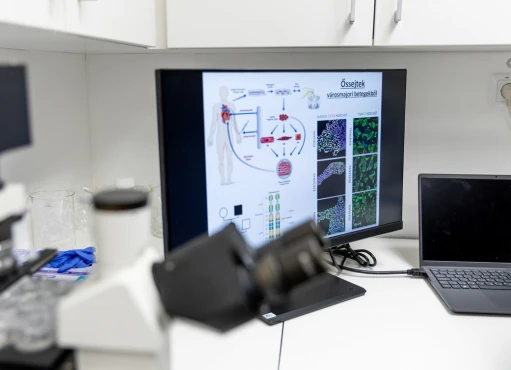
The aorta is the largest artery in the human body. It carries blood from the heart to all tissues and organs of the body and is divided into ascending, arc and descending. The latter is also divided into two parts: chest and abdominal.
Classification of aortic aneurysm
There are several classifications of this pathology, which can be divided into 5 groups:
- By etiology (origin) - as a result of atherosclerotic or degenerative damage (for example, with Marfan syndrome), as well as after an inflammatory process and trauma;
- In shape - baggy and fusiform (more common);
- By the structure of the wall - real and pseudo-wall (the wall is formed by adventitia with the surrounding tissues after the rupture of the inner and middle membranes; most often post-traumatic)
- According to the clinical picture - asymptomatic, symptomatic, discontinuous course;
- By location - chest - located in the chest cavity (often localized in the ascending part of the aorta), abdominal - located below the diaphragm, thoracoabdominal aneurysm.
Symptoms of the disease
A thoracic aortic aneurysm most often has no manifestations. The first symptom of pathology may be an embolic event - stroke, ischemia of the lower extremities or intestines, kidney infarction, etc.
The clinical manifestations and the natural course of this disease depend on their location. The average growth rate of thoracic aneurysms is 0.1-0.2 cm per year. Pathology associated with Marfan syndrome or aortic dissection may expand at a faster rate. The risk of rupture is related to the size of the aneurysm and the presence of symptoms.
As noted earlier, most thoracic aortic aneurysms are asymptomatic, but compression or damage to adjacent tissues by a dilated vessel can cause symptoms such as chest pain, shortness of breath, cough, hoarseness, and dysphagia (difficulty swallowing). Dilation of the ascending aortic aneurysm can cause congestive heart failure, and compression of the superior vena cava can cause congestion of blood in the head, neck, and upper extremities.
Diagnosis of the disease
A chest x-ray is usually the first diagnostic test that can prompt a doctor to diagnose a thoracic aortic aneurysm. During its implementation, the following can be identified:
- expansion of the shadow of the mediastinum;
- displacement or compression of the trachea or the left main truncal bronchus.
Echocardiography, especially transesophageal echocardiography, can be used to evaluate the proximal (located closer to the heart) of the ascending aorta and the descending thoracic aorta. However, in general, ultrasound (the type of which is echocardiography) is the main method for diagnosing abdominal aortic aneurysms.
CT angiography allows you to accurately assess the size (with an accuracy of 0.2 cm) and the length of the aneurysm, the anatomical relationship between the aneurysm and adjacent organs, as well as arteries extending from the aorta (sometimes this is sufficient for a preoperative assessment of the patient).
MR angiography is also used to assess the size and extent of the aneurysm if CT angio cannot be performed. This method is especially justified in the framework of serial follow-up examinations carried out in younger patients. MR angiography is less commonly used in acute conditions.
Intravascular ultrasound - allows you to get an image of the aortic wall from the inside by introducing ultrasound sensors through a catheter.
In asymptomatic patients whose aneurysms are too small to warrant surgery, non-invasive (atraumatic) contrast-enhanced CT or MRI testing is usually done at least every 6 to 12 months to monitor the disease.
Even if an aneurysm is found in a patient at any level, the doctor usually recommends performing an examination of the entire aorta in order to exclude coexisting pathology. In addition to this, the possibility of ultrasound examination (Doppler) of the peripheral arteries for aneurysms is being considered. It is also recommended to rule out aortic valve abnormalities (usually by echocardiography).
Who may be at increased risk of developing a thoracic aortic aneurysm?
The risk of this pathology is higher in:
- people aged 65 and over;
- people who use tobacco;
- patients with arterial hypertension (high blood pressure damages the blood vessels in the body, increasing the likelihood of developing aneurysms and other vascular diseases);
- patients with atherosclerotic damage to the vascular bed, obesity and lipid imbalance (dyslipidemia);
- people whose blood relatives had an aneurysm (regardless of its location);
- patients with Marfan syndrome and bicuspid aortic valve. Nearly half of those with an aortic valve with two cusps instead of three may develop an aortic aneurysm.
Thus, an aneurysm of the thoracic aorta is a pathological expansion of this vessel in the chest cavity. This pathology is usually discovered by chance based on the results of imaging tests (X-ray, MRI, CT) performed for other indications. Contrast-enhanced CT, magnetic resonance imaging (MRI), and conventional invasive aortography are sensitive and specific tests for assessing thoracic aortic aneurysms and branch lesions.
References:
- Salameh, M. J., Black, J. H., & Ratchford, E. V. (2018). Thoracic aortic aneurysm. Vascular Medicine, 1358863X1880776. doi:10.1177/1358863x18807760
- Harrison`s Principles of Internal Medicine 19/E (Vol.1). Dennis Kasper, Anthony Fauci, Stephen Hauseret all. McGraw-HillEducation 2015 ISBN: 0071802134 ISBN-13(EAN): 9780071802130.
- Interna szczeklika - duży podręcznik. Medycyna praktyczna. 2021. ISBN 9788374306522.
- 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. (2014). European Heart Journal, 35(41), 2873–2926. doi:10.1093/eurheartj/ehu281.