Definition
Left ventricular failure is a clinical syndrome characterized by a sharp decrease in cardiac output and stasis in the small circle of blood circulation. The disease occurs in myocardial infarction and other cardiac emergencies, other somatic pathologies, and poisoning with cardiotoxic substances. It is clinically manifested by pulmonary edema and cardiogenic shock. For diagnosis, ECG and echocardiography, chest X-ray, coronarography, and laboratory tests are used. Treatment of heart failure includes oxygen therapy and drug support; surgical methods are prescribed when indicated.
General information
Acute heart failure is the main cause of hospitalization and mortality of patients with cardiovascular pathologies worldwide. The disease is characterized by a severe course, rapid decompensation, and increasing multiorgan disorders, which require emergency comprehensive, multidisciplinary care from physicians. Left ventricular HF represents a severe problem for the healthcare economy: the costs of its treatment account for about 2% of all medical expenses.
Causes
Acute left ventricular failure occurs as a decompensated variant of chronic HF, as well as in patients without previous heart disease. In older adults, the main cause of heart failure is ischemic heart disease, which causes up to 60-70% of all cases of critical circulatory disorders. Among the etiologic factors of the disease also distinguish the following:
- Non-inflammatory heart disease. In young and middle-aged patients, many cases of acute left ventricular failure are associated with dilated cardiomyopathy, rhythm disturbances (fibrillation, ventricular tachycardia), and heart defects.
- Emergency conditions. The causes of acute circulatory disorders are cardiac tamponade, rupture of aortic aneurysm, and pulmonary embolism. Left ventricular failure is considered a typical manifestation of a complicated form of hypertensive crisis.
- Myocarditis. In severe inflammation of the myocardium, its contractility is sharply reduced, and cardiac output falls, which is a trigger factor for HF. Myocarditis more often has an infectious-allergic character; occasionally, it is caused by toxic, autoimmune factors.
- Non-cardiac causes. Disturbances in the small circulation circle are provoked by background diseases: cerebral blood flow disorders, bronchial asthma, and renal failure. HF may occur with severe drug or alcohol intoxication.
- Cardiotoxic substances. Sudden cardiac dysfunction is observed, in poisoning with organophosphorus compounds (OPs) and insecticides.
Classification
According to the phase of cardiac dysfunction, left ventricular failure can be systolic (cardiogenic shock) when there is low blood flow in the large circle and diastolic (pulmonary edema), for which stasis in the veins of the small circle is typical. In modern cardiology, to determine prognosis and treatment tactics, the classification of "clinical severity" is used, which includes four classes:
- Class I - "warm and dry" patients. Low cardiac output with normal blood supply to peripheral tissues and absence of stasis in the small circle.
- Class II - "warm and moist." HF with blood deposition in the venous channel of the lungs and absence of symptoms of peripheral hypoperfusion.
- Class III "cold and dry." Disorders of arterial blood supply in the covering tissues without symptoms of pulmonary congestion.
- Class IV - "cold and wet." The most severe variant of acute left ventricular failure, in which tissue hypoperfusion is combined with signs of pulmonary edema.
Killip T. (1967) classification, according to which HF is divided into four stages according to the severity of clinical manifestations, is also used for diagnosis in cardiologic practice. When assessing patients' conditions, according to the Forrester method, systolic index (SI) less than 2.2 l per minute per 1 m<sup>2</sup> body area and an increase in pulmonary artery wedge pressure (PAWP) of more than 18 mm Hg are taken into account.
Symptoms of left ventricular failure
The clinical picture of the disease consists of separate syndromes and depends on the variant of HF. Signs of congestion in the small circle are severe dyspnea and audible at a distance respiratory wheezes, which persist at rest. To alleviate the condition, patients sit down and rest on their arms (orthopnea), but suffocation is present even in this position. When coughing and breathing, frothy pinkish sputum comes out of the mouth.
Disorders of peripheral blood supply manifest as severe weakness, dizziness, and pre-syncope. The skin becomes pale with a grayish tint, and distal parts of the limbs and nasolabial triangle acquire a cyanotic color. The patient has a thready pulse, sharply decreased blood pressure, and decreased volume of urination.
If left ventricular failure occurs as a result of acute coronary syndrome, the person is bothered by severe pain behind the sternum, which irradiates to the left shoulder blade, neck, and left arm. The pain syndrome can be so intense that the patient loses consciousness from shock. In severe HF, cardiopulmonary and multiorgan failure increases, and sopor or coma develops.
Diagnosis
Patients are examined by intensive care unit physicians together with cardiologists. By assessing the clinical condition and physical manifestations, it is possible to determine the severity of acute left ventricular failure. Further diagnosis is carried out in parallel with emergency measures to stabilize the patient's condition. The following methods of research are used:
- Cardiac ultrasound. This study reveals a decrease in ejection fraction, disorders of the structure and function of the heart's valve apparatus, and signs of effusion in the pericardial bag. Doppler ultrasound assesses blood flow in the heart cavities and main vessels.
- Electrocardiogram. The ECG determines the heart rhythm and identifies some etiologic factors of HF: myocardial infarction, fibrillation, and tachycardia.
- Coronary angiography. An invasive method of investigation with contrast is needed to detect blood clots, ischemia, and other coronary blood flow disorders. To clarify the diagnosis, CT angiography of the venous arteries and large vessels of the bronchopulmonary system is used.
- Radiography. X-rays show the degree of dilation and deformation of the contours of the heart and the presence of congestion in the lungs. For a more accurate determination of the interstitial type of pulmonary edema, ultrasound is used.
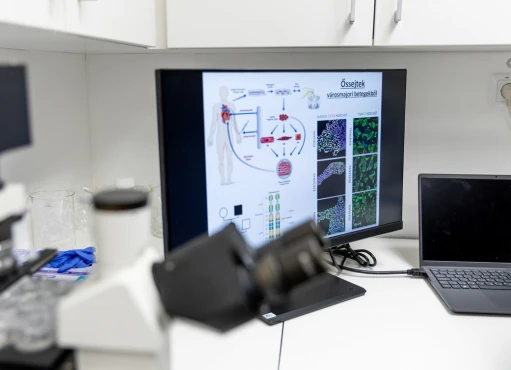
- Laboratory tests. The standard diagnostic complex includes clinical blood and urine tests, blood biochemical analysis, and coagulogram. To confirm the cardiac etiology of acute left ventricular failure, natriuretic peptide, myocardial markers, and acute phase proteins are measured.
Treatment of acute left ventricular failure
Conservative therapy
Intensive therapy aims to stabilize hemodynamics as soon as possible and eliminate symptoms. The best long-term prognosis is observed when treatment is started within the first 2 hours from the onset of HF signs. Assistance is provided in intensive care, and the patient is subsequently transported to a cardiac hospital when the condition improves. Extended cardiorespiratory monitoring is mandatory.
The key task in acute left ventricular failure is to restore tissue oxygenation to stop the cascade of pathophysiological processes and multiorgan disorders. Oxygen therapy through nasal cannulas or face masks is prescribed in moderate hypoxemia. When indicated, non-invasive ventilation in the CPAP mode is artificial ventilation of the lungs. In parallel, medications of the following groups are prescribed:
- Opioid analgesics. The drugs control pain syndrome in myocardial infarction, promote vasodilation, suppress dyspnea, and stabilize the condition of patients with pulmonary edema.
- Vasodilators. Nitrates, which have a rapid clinical effect, are used to correct peripheral hypoperfusion syndrome. ACE inhibitors are used for specific indications, but their role still needs more study.
- Diuretics. Medications are prescribed in the presence of fluid stasis in the small circle and in the absence of severe renal dysfunction. Loop diuretics, which have an additional vasodilating effect, are most often used to reduce resistance in pulmonary vessels.
- Inotropic drugs. Drugs are prescribed in all cases of deterioration of peripheral circulation. This group's classic representatives are dopamine and dobutamine, cardiac glycosides.
- Anticoagulants. Medications are prescribed to all patients with acute coronary syndrome, arrhythmias, pulmonary embolism, and other conditions with a high risk of recurrent thrombosis.
Surgical treatment
Cardiac surgeons are required for patients who cannot achieve sustained clinical improvement by conservative methods. Surgical intervention is performed for emergency myocardial revascularization, reconstruction of the valve apparatus, and treatment of aortic aneurysm or aortic dissection. In severe acute left ventricular failure forms, mechanical circulatory support (ECMO, intra-aortic balloon pump, LVAD implantation) is used.
Prognosis and prevention
Acute left ventricular failure is characterized by a severe prognosis and, in the absence of emergency care, often ends in the death of the patient. Successful implementation of intensive care measures should be accompanied by long-term inpatient and outpatient treatment by a cardiologist to eliminate the negative consequences of HF and control the diseases that cause it.
Measures to prevent heart failure are limited to the prevention and early diagnosis of cardiovascular diseases. Non-specific advice includes an active lifestyle, limiting fats and alcohol in the diet, and avoiding stressors. All people over 40 should have an annual health check-up with a visit to a general practitioner (or cardiologist) and a standard set of tests.