Introduction
Myocardial infarction, a severe form of ischemic heart disease, arises when the blood supply to the myocardium, which makes up most of the heart’s mass, is significantly reduced or stopped.
About a disease
This disruption leads to the death of numerous heart cells, impairing the heart’s functionality and consequently affecting the overall blood supply system. Such an event results in tissue and organ oxygen deprivation, potential suffocation, brain dysfunction, and in extreme cases, may lead to cardiac arrest.
Myocardial infarction is a critical condition that results in permanent damage to the heart. It is most common in individuals over 50, with around 60% of people aged 65 and above having experienced a heart attack. Nevertheless, younger individuals are not exempt from the risk.
Immediate medical attention is crucial when myocardial infarction symptoms first appear. Calling for an ambulance right away is essential in handling this potentially life-threatening situation.
Symptoms of myocardial infarction
The manifestations of the disease are individual and depend on the extent of myocardial necrosis, the stage of infarction and the overall state of the cardiovascular system. In diabetics, the attack may be painless at all.
The following stages of myocardial infarction and their characteristic symptoms are distinguished:
- Pre-infarction state. It is observed in about 45% of patients, in the rest the disease begins suddenly. This period is characterized by repeated attacks of angina pectoris, accompanied by severe pain behind the sternum. The general condition changes – the psychoemotional background decreases, there is a feeling of brokenness and fear. Drugs to control angina attacks reduce their effectiveness at this stage.
- The acute phase of a heart attack. It may last from half an hour to several hours. The patient experiences the strongest burning, pressing (angina) pain behind the sternum, radiating to the left side of the body (arm, forearm and shoulder, clavicle, interscapular region, scapula, thigh). The pain peaks in a few minutes and then persists in a wavy pattern for an hour or longer.
- Acute period. Persists for up to 2 days. Recurrences of up to 10 days or longer are possible. At this stage, pressure pain usually subsides. Heart rhythm disturbance, decreased blood pressure persist. If the anginal pain does not recede, it indicates a prolonged course of infarction or a complication in the form of inflammation of the serous membrane of the heart (episthenocardial pericarditis).
- Subacute period. It can last up to a month and is characterized by general improvement of well-being, normalization of body temperature, restoration of respiration, heart rhythm.
- Postinfarction state. This is the final stage of the acute phase, which can last up to 6 months. In place of tissue areas affected by necrosis, a dense scar is formed. In general, the condition stabilizes, the clinical manifestations of the disease go away, laboratory and physical parameters are restored to normal values. In case of extensive myocardial damage, heart failure may persist.
Myocardial infarctions are also classified into two types based on the findings in an electrocardiogram (ECG): ST-Elevation Myocardial Infarction (STEMI) and Non-ST-Elevation Myocardial Infarction (NSTEMI). This classification is crucial for determining the appropriate treatment strategy and has implications for the patient’s prognosis.
STEMI (ST-Elevation Myocardial Infarction)
STEMI is characterized by the elevation of the ST segment on an ECG, indicating a full-thickness (transmural) infarction of the heart muscle. This type of MI typically results from a complete blockage of one of the heart’s major arteries. The ST segment elevation is a direct indicator of acute injury to the heart’s muscle cells and requires immediate treatment to restore blood flow and minimize heart damage. Treatment options include percutaneous coronary intervention (PCI) — the preferred method for its ability to quickly reopen the blocked artery — or thrombolytic therapy if PCI is not available within the critical first hours after the onset of symptoms.
STEMI is one of the most relevant heart diseases, that is why you can find more than 750 hospitals around the world, that treat this condition (https://doctor.global/results/diseases/acute-st-elevation-myocardial-infarction-stemi).
NSTEMI (Non-ST-Elevation Myocardial Infarction)
NSTEMI is identified by changes in biomarkers (such as troponin) that indicate heart muscle damage without the ST segment elevation on an ECG. It usually reflects a partial thickness (subendocardial) infarction of the heart muscle, often due to a partial blockage or temporary complete blockage of a coronary artery. Patients with NSTEMI may have a slightly better short-term prognosis than those with STEMI, but they still require urgent assessment and management. The initial approach to managing NSTEMI involves medical therapy to stabilize the patient, followed by diagnostic evaluation using coronary angiography to determine whether coronary artery revascularization with PCI or coronary artery bypass grafting (CABG) is needed.
The distinction between STEMI and NSTEMI is essential for guiding immediate treatment decisions. Both conditions are considered acute coronary syndromes (ACS) and represent a spectrum of the same disease process, with the primary difference being the extent and location of the myocardial damage. Regardless of the type, prompt medical attention and treatment are critical to improving outcomes and reducing the risk of further cardiac events and complications.
Causes of myocardial infarction
The main causes of myocardial infarction are atherosclerosis and spasm of the coronary arteries, causing narrowing of their lumen.
In addition, predisposing factors to the development of the disease may include:
- thrombosis in blood clotting disorders (coagulopathies);
- diabetes;
- hypertensive crisis;
- obesity;
- excessive physical exertion and psychoemotional stress against the background of ischemic heart disease and angina pectoris;
- alcohol and tobacco abuse.
Diagnosis of myocardial infarction
If symptoms of myocardial infarction occur, the patient is urgently hospitalized for urgent diagnosis and first aid. If the diagnosis is confirmed, the patient is hospitalized by an ambulance crew to a specialized municipal medical center.
Methods of diagnosis of myocardial infarction:
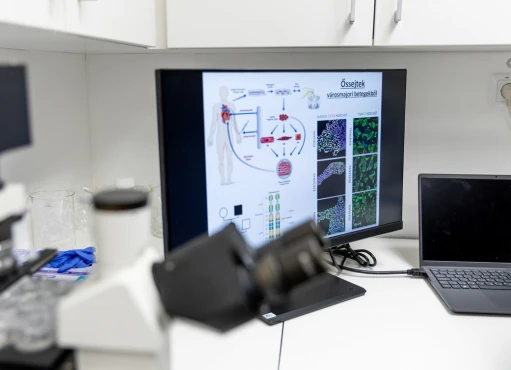
- Laboratory examinations: blood analysis, general, biochemical and for cardiotropic proteins (MB-CFC, AsAT, LDH-1, troponin).
- Instrumental studies: ECG, computer tomography, MRI, angiography, coronography, ultrasound of the carotid arteries.
Treatment methods for myocardial infarction
At the pre-hospital stage, drug therapy is performed to stabilize the patient’s condition and reduce the risk of mortality:
- Restoration of coronary blood flow. It is carried out in the first day after the development of infarction by administering special drugs that quickly dissolve blood clots.
- Control of pain syndrome. It is carried out with analgesics in combination with neuroleptics and intravenous nitroglycerin (in case of high blood pressure).
- Elimination of arrhythmia, heart failure, cardiogenic shock, normalization of blood coagulation. To do this, prescribe: lidocaine, atenolol, verapamil, magnesia, nitrates, heparin, acetylsalicylic acid, antispasmodics, etc.
In case of heart vessel damage detected at the diagnostic stage, surgery is performed.
- Balloon endovascular angioplasty with stenting. It is performed urgently in the first hours after diagnosis of a heart attack in order to restore vascular patency. The operation makes it possible to promptly eliminate the cause of vasoconstriction and prevent negative consequences of atherosclerotic lesions. During the operation, a stent is placed inside the vessel to normalize blood flow in the coronary arteries. This makes it possible to effectively restore the narrowed lumen of the vessel and avoid possible recurrence of the disease.
- Coronary bypass surgery. In cases when for one reason or another stenting of the coronary arteries is impossible, surgeons may decide to perform open heart surgery to bypass the arteries affected by atherosclerosis. The patient’s own vessels – great saphenous veins, internal thoracic and radial arteries – are used as shunts.
Prevention of myocardial infarction
Anyone who has problems with the cardiovascular system, should take care of the prevention of myocardial infarction in a timely manner.
Methods of preventing the disease:
- Maintaining an adequate level of physical activity. It is important to lead a mobile lifestyle in which the heart muscle will receive adequate exercise and training.
- Refusal from bad habits (alcohol and tobacco). Excessive addiction to drugs in the form of tobacco and alcohol contributes to the narrowing and blockage of blood vessels, clogging the body with toxins, which has a detrimental effect on the heart.
- Healthy diet. Avoid fatty and spicy foods and eat plenty of protein, raw vegetables and fruits.
- Regular consultations with a cardiologist. After the age of 40, it is recommended to have regular medical check-ups, including ECG examinations.
Recovery and Rehabilitation
Recovery from an MI involves careful management of heart health. This includes:
- Cardiac Rehabilitation: A structured program of exercise and education.
- Lifestyle Changes: Adopting a heart-healthy diet, quitting smoking, and managing stress.
- Regular Medical Check-ups: Monitoring heart health post-MI is vital.
Conclusion
Myocardial infarction is a serious medical condition that requires immediate attention. Understanding the causes, symptoms, and treatment options is vital for prompt action, which can be life-saving. Embracing a heart-healthy lifestyle and regular medical check-ups play a pivotal role in preventing heart attacks. Remember, the key to combating MI lies in prevention, early detection, and prompt, effective treatment.