Classification, pathophysiology of Ebstein anomaly
Ebstein anomaly includes a wide range of morphological and clinical manifestations. Those who show symptoms in early infancy tend to be at the highest risk. This pathology affects the tricuspid valve (its other name is tricuspid) and is a congenital malformation of the cardiovascular system. At the same time, there is a shift of the point of attachment of the cusps of this valve - septal and posterior - down. However, the anterior cusp is usually not affected. The leaflets themselves are dysplastic, i.e. developed incorrectly. As a result of the displacement, poor closure of the valve leaflets (in other words, impaired coaptation) is observed, which leads to tricuspid regurgitation - the backflow of blood through the tricuspid valve. This, in turn, causes an increase in the size of the right atrium of varying degrees.
Causes and prevalence of Ebstein anomaly
No defect in any one gene has been identified with Ebstein anomaly. This pathology appears to be genetically heterogeneous; develops as a result of various, unpredictable, several gene anomalies. Several candidate genes have been proposed as culprits, including GATA4 and NKX2.5. Lithium exposure during pregnancy has been reported as a causative factor.
Ebstein anomaly accounts for 0.3 to 0.6% of all congenital heart defects. There is no preponderance towards children of any gender, and most cases are completely sporadic, i.e. occur spontaneously and randomly. The frequency of recurrence in the offspring of women is higher (6%) than in the offspring of men (0.6%).
Anatomy and pathophysiology of Ebstein anomaly
The tricuspid valve separates the right atrium (the chamber that receives blood from the body) from the right ventricle (the chamber that pumps blood to the lungs).
In Ebstein anomaly, the two leaflets of the tricuspid valve move down into the pumping chamber. The third flap has an elongated shape and can be attached to the chamber wall. In rare cases, the valve becomes so deformed that it does not allow blood to flow freely forward in the normal direction.
Most often, these anomalies cause blood to leak through the tricuspid valve from the right ventricle back into the right atrium, into the systole - i.e. when the muscles of the right ventricle contract. As a result, the right atrium expands in size, accommodating an unusually large volume of blood.
Hemodynamic disturbances depend on the severity of the lesion. The main determining factors are the degree of displacement of the tricuspid valve leaflets and the degree of tricuspid regurgitation. With a mild degree of Ebstein anomaly, the function of the tricuspid valve is close to normal. But if the tricuspid regurgitation is severe enough, with each atrial contraction blood is ejected into the right ventricle, and with ventricular contraction it is pushed back into the right atrium. This can lead to congestive heart failure.
Normally, the fetus has a communication between the right and left atria, known as the foramen ovale (foramen ovale). It usually closes after the baby is born. However, in Ebstein anomaly, there is a reverse flow of blood into the right atrium, so the pressure inside this chamber of the heart becomes very high. This keeps the foramen ovale open, and as a result, oxygen-poor blood flows from the right atrium to the left, bypassing the lungs and heading straight for the organs and tissues. This is why children with Ebstein anomaly may have a bluish, or "cyanotic" skin tone.
This heart disease can also occur with other lesions of this organ, such as stenosis or atresia of the pulmonary valve, atrial or ventricular septal defect. In addition, many patients with Ebstein anomaly have an extra conduction pathway in the heart that can potentially lead to episodes of an abnormal fast heart rate called supraventricular tachycardia (this condition is known as Wolff-Parkinson-White syndrome).
Signs and symptoms of Ebstein anomaly
Ebstein anomaly can range from very mild to very severe, having 4 degrees, from 1 to 4, respectively. Many patients with milder forms of Ebstein anomaly are asymptomatic, and as a result, the malformation may be discovered in adulthood—often due to the discovery of a heart murmur. Abnormal or extra heart sounds may also be detected during a routine examination.
In some infants and children, the skin turns bluish (cyanotic) due to blood flow from the right atrium to the left. Children may complain of heart palpitations and skipping beats, sometimes people describe this feeling as "a strange heartbeat". They are characterized by increased fatigue, shortness of breath, especially during the game, and chest pain. Growth and development in patients with Ebstein anomaly is usually normal.
Severely affected children are often critically ill at birth, with low oxygen saturation and heart failure requiring immediate intensive care.
Diagnosis of Ebstein anomaly
If you suspect a heart defect, you should immediately consult a doctor. A chest x-ray should be done to assess size. Often the diagnosis of Ebstein anomaly is suspected precisely because of a very large heart on a chest x-ray.
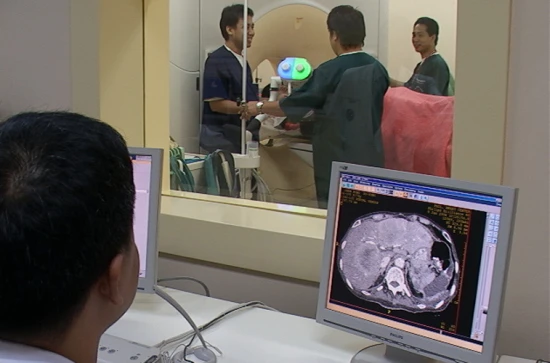
Echocardiography is used to definitively diagnose Ebstein anomaly and identify any associated heart defects. This study allows the pediatric cardiologist to determine the degree of valve wall displacement, the severity of valve failure, or orifice narrowing. You can determine the size of the chambers of the heart and the presence of an open foramen ovale.
An electrocardiogram records the electrical activity of the heart. It is indicated for recording the heart rhythm when there is a violation of it. An exercise stress test may be performed to better assess heart function during increased activity. Some patients with abnormal heart rhythms may require an additional electrophysiological study to more accurately identify problems with the heart rhythm.
Invasive diagnostic tests are used much less frequently today than in previous years. This is due to the availability of more informative non-invasive methods, such as echocardiography and MRI. However, some patients with Ebstein anomaly may require cardiac catheterization.
Treatment of Ebstein anomaly
Mild defects often do not require special treatment. In addition, there is no need for bacterial endocarditis prophylaxis, such as taking antibiotics during dental visits. Drug treatment is reserved for children with congestive heart failure or abnormal heart rhythms.
Surgery may only be indicated under certain circumstances. Surgical repair or replacement of the tricuspid valve and closure of the foramen ovale are sometimes recommended. Surgery may be indicated for older children with moderate to severe congestive heart failure, significant enlargement of the heart, cyanosis, or abnormal blood clots. Abnormal accessory pathways that contribute to supraventricular tachycardia may be removed.
Medical therapy for heart failure or arrhythmias is usually combined with elective surgery. Very severe forms of Ebstein anomaly may require surgery in the neonatal period, and management is more similar to that for children with single ventricular heart anomalies.
Disease prognosis
Without any treatment, the prognosis for children with Ebstein anomaly is very poor. Studies have shown that only half of all people affected by this disease, without treatment, can live up to 13 years. However, people with milder forms have a better prognosis and life expectancy close to the population average.
The Zelermeier index is used to predict outcome based on the fetal or neonatal echocardiogram. This indicator allows you to predict the likelihood of mortality. The higher the class, the higher this indicator:
- at grade 1 (ratio less than 0.5), the mortality rate is 0%;
- at grade 2 (ratio 0.5 to 0.99), the mortality rate is 10%;
- at grade 3 (ratio 1.0 to 1.49), the mortality rate is 4%;
- at grade 4 (coefficient greater than 1.5), the mortality rate is 100%.
Life of people with Ebstein anomaly
Ebstein anomaly can be diagnosed at any age, including adults. As already mentioned, people with the mildest form of the disease may not have any problems throughout their lives. Many people with this pathology develop arrhythmia, and the older the person, the higher the likelihood of such an outcome.
All people with Ebstein anomaly need lifelong medical supervision. Many needs treatment for rhythm disturbances, including ablation procedures. Episodes of life-threatening arrhythmias tend to recur; in addition, the development of other arrhythmias that require constant monitoring is possible.
References:
- Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM. Cyanotic congenital heart lesions: lesions associated with decreased pulmonary blood flow. In: Kliegman RM, St.Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 457.
- Webb GD, Smallhorn JF, Therrien J, Redington AN. Congenital heart disease in the adult and pediatric patient. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 75.
- Mulla S, Asuka E, Siddiqui WJ. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 28, 2021. Tricuspid Regurgitation.
- Voges I, Al-Mallah MH, Scognamiglio G, Di Salvo G. Right Heart-Pulmonary Circulation Unit in Congenital Heart Diseases. Heart Fail Clin. 2018 Jul;14(3):283-295.