Definition
Arrhythmogenic right ventricular dysplasia (cardiomyopathy) is a disease of presumably genetic nature characterized by structural changes in the right ventricle and the development of arrhythmias. The course varies from asymptomatic forms to forms with marked tachyarrhythmias, extrasystole, cardialgia, and heart failure. Diagnosis is made with the help of echocardiographic, electrocardiographic, magnetic resonance studies, and myocardial biopsy. There is no specific treatment; therapy is reduced to the elimination of arrhythmia and congestive heart failure. If there is no effect of drug therapy, implantation of a cardioverter-defibrillator is used.
General information
Arrhythmogenic right ventricular cardiomyopathy (arrhythmogenic right ventricular dysplasia, arrhythmogenic right ventricular disease) is a disease affecting the wall of the right ventricle, in which pathologic foci of fatty and fibrinous infiltration are formed in the thickness of the myocardium, sometimes with inflammation (myocarditis). The incidence in different regions varies within 1-6:10000 inhabitants; among the detected patients, the overwhelming majority are men under 40 years of age, and the sex distribution is 4:1. It tends to be inherited, so currently, most forms of arrhythmogenic dysplasia are defined as an autosomal dominant disease with incomplete penetrance. Interest in the disease has increased dramatically due to the identification of its role in the development of sudden cardiac death. Thus, histologic studies of myocardium in children and adolescents under 20 years of age whose cause of death was cardiovascular pathology showed that changes associated with arrhythmogenic dysplasia were found in 26% of cases.
Causes
Because of the heterogeneity of the disease manifestations, there is no universally recognized point of view on the causes of arrhythmogenic dysplasia. It is possible that arrhythmogenic right ventricular dysplasia combines several similar pathologies with different etiologies. However, the only documented theory to date is hereditary, which explains the occurrence of arrhythmogenic right ventricular cardiomyopathy through a genetic mutation.
Disturbances in the structure of different proteins lead to decreased resistance of cardiomyocytes to damaging factors, which leads to fatty infiltration over time. However, disruption of desmosome protein functions plays the main role in the development of arrhythmias in arrhythmogenic dysplasia, altering the spread of excitation through the myocardium.
In some cases, instead of focal fatty infiltration of the right ventricular walls, fibrinous infiltration occurs. This infiltration is inflammatory in nature and generally resembles the picture in viral myocarditis caused by Coxsackie virus and others. This form tends to spread to the left ventricle and is characterized by a severe course, often leading to the patient’s death.
Most mutations are inherited in an autosomal dominant pattern with a 30-50% penetrance. One extremely rare form of arrhythmogenic right ventricular cardiomyopathy (Naxos disease – only 25 cases have been described) is autosomal recessive and has a high penetrance of more than 90%. Homozygotes for the mutant gene suffer from malignant ventricular arrhythmias and often die in childhood or adolescence.
Classification
Due to the pronounced heterogeneity of clinical forms of arrhythmogenic cardiomyopathy, attempts to systematize and classify the types of this disease have been repeatedly accepted. Currently, the following types of arrhythmogenic right ventricular cardiomyopathy are distinguished:
- Primary form.
- Naxos disease is characterized by autosomal recessive inheritance and malignant ventricular arrhythmias.
- Venous cardiomyopathy – often extends to the wall of the left ventricle, has a solid hereditary character (penetrance of about 50%), and patients may die in childhood.
- Tachycardia is caused by a focus of excitation in the right ventricle without extrasystoles or manifestations of heart failure.
- Rare ventricular extrasystoles are caused by a focus of excitation in the right ventricular wall associated with an area of inflammation. This form of dysplasia may be complicated by fatal myocarditis.
- Uhl’s anomaly is a rare form of arrhythmogenic dysplasia characterized by increasing heart failure and death. Histologic examination of the heart reveals complete replacement of cardiomyocytes by fatty and fibrinous tissue.
- Non-arrhythmogenic form – in most cases, does not manifest itself; it is associated with asymptomatic cases of sudden cardiac death.
Symptoms of arrhythmogenic cardiomyopathy
Clinical forms of arrhythmogenic dysplasia are divided into four main groups. In the asymptomatic form, the pathology does not manifest itself in any way during the patient’s life, including electrocardiographic studies. The arrhythmic form is characterized by the development of tachyarrhythmias, ventricular extrasystole, and the appearance of other electrocardiographic signs. Subjective symptoms are usually absent. With the development of a pronounced clinical formagainst the background of tachyarrhythmias, cardialgia, attacks of palpitations, and dizziness occur. The most severe type of clinical manifestation of arrhythmogenic cardiomyopathy is the development of heart failure on the right ventricular type with a characteristic symptom complex – venous stasis, edema, and ascites. At the same time, heart failure can occur against the background of heart rhythm disturbance or without it.
In some cases, these groups reflect the stages of development of disorders caused by arrhythmogenic right ventricular cardiomyopathy. However, in some patients, the development of pathology may last for years, while in others, it may take less than a month from asymptomatic form to heart failure. In addition, any of the forms or any stage of arrhythmogenic cardiomyopathy can be fatal due to ventricular fibrillation, Uhl’s anomaly, or lightning viral myocarditis.
Diagnosis
For the diagnosis of arrhythmogenic right ventricular dysplasia in practical cardiology, the full range of modern techniques of cardiac function testing is used:
- Cardiac ultrasound. Echocardiography determines the ventricular end-diastolic dimension (EDD) and end-systolic dimension (ESD) and compares these data. If the ratio of the right ventricular EDD to the left ventricular ESD is 0.5 or more, this indicates the presence of arrhythmogenic dysplasia.
- ECG. ECG signs of arrhythmogenic right ventricular cardiomyopathy include ventricular complex prolongation of more than 110 ms on lead V1, epsilon wave on the ST segment in leads V1-V3, T inversion in thoracic leads due to delayed depolarization of the right ventricle, as well as the presence of tachyarrhythmias and ventricular extrasystoles.
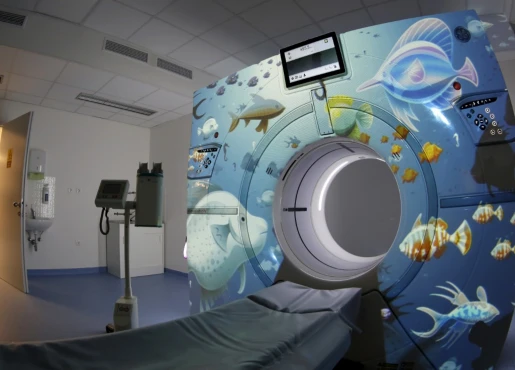
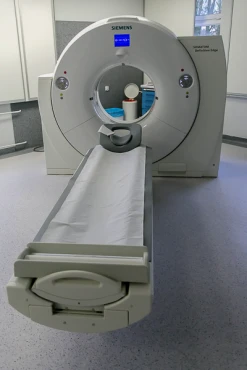
- X-ray. On X-ray contrast ventriculography, right ventricular dilatation can be detected, and in some cases, a bulge (aneurysm) in the area of the myocardial fibrolipotic dysplasia focus is directly visualized. In recent years, magnetic resonance imaging with gadolinium contrast has been used for specific diagnosis of arrhythmogenic dysplasia, which allows not only to obtain a three-dimensional image of the heart but also to differentiate fatty and fibrinous foci from unchanged myocardium.
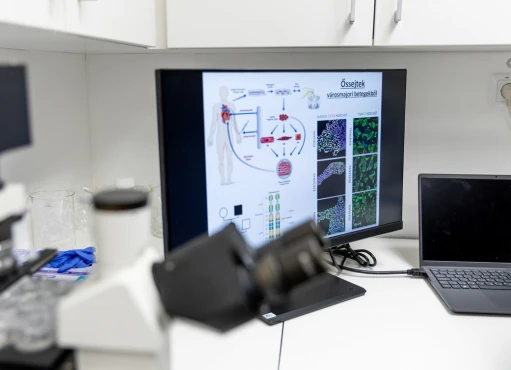
- Myocardial biopsy. To clarify the diagnosis, myocardial biopsy with the subsequent histological study of tissues is practiced – in arrhythmogenic dysplasia, fatty infiltration, changes in the color and shape of desmosomes, and a decrease in their number will be observed.
An important feature is the familial nature of the symptoms or the presence of relatives who have died of sudden cardiac death or ventricular fibrillation. In this case, the diagnosis is confirmed by a genetic diagnosis. Differential diagnosis is made with idiopathic forms of ventricular tachyarrhythmias.
Treatment
Drug treatment of arrhythmogenic dysplasia includes antiarrhythmic drugs. Reducing the severity of tachyarrhythmias plays an essential role in preserving the patient’s life; the cardiologist controls the effectiveness of drugs with the help of Holter monitoring. In cases where drug therapy is ineffective, resort to implantation of a cardioverter-defibrillator or pacemaker. If heart failure develops, ACE inhibitors and beta-blockers are used.
Surgical treatment for ARVD is considered when patients are refractory to medical therapy or when they have a high risk of sudden cardiac death. The primary goals are to prevent arrhythmic events, manage heart failure symptoms, and improve the quality of life.
Surgical Options
- Implantable Cardioverter-Defibrillator (ICD): The most common surgical intervention for ARVD is the implantation of an ICD. This device monitors heart rhythm and delivers electric shocks to restore a normal heartbeat when dangerous arrhythmias are detected. It is highly effective in preventing sudden cardiac death.
- Cardiac Ablation: In cases where arrhythmias are frequent and debilitating, catheter ablation may be used. This procedure involves threading a catheter through the blood vessels to the heart to destroy small areas of tissue where abnormal heartbeats are triggered.
- Right Ventriculotomy or Ventricular Tachycardia Ablation: In select cases, especially when arrhythmias originate from specific areas of the right ventricle, a surgical approach might be necessary to remove or ablate the arrhythmogenic tissue directly.
- Heart Transplantation: In advanced stages of ARVD, where both ventricles are significantly affected and the patient has severe heart failure, heart transplantation may be considered as a last resort.
Prognosis and prevention
The prognosis is uncertain because of the high variability of arrhythmogenic dysplasia manifestations. Fatal ventricular fibrillation can occur at any time, especially if untreated. With regular antiarrhythmic therapy, the risk of fatal outcomes is reduced by about one-third. The best results are shown by the combination of pacemakers and drug therapy, which reduces the risk of fatal fibrillation to almost zero. When heart failure develops, the prognosis is usually unfavorable.